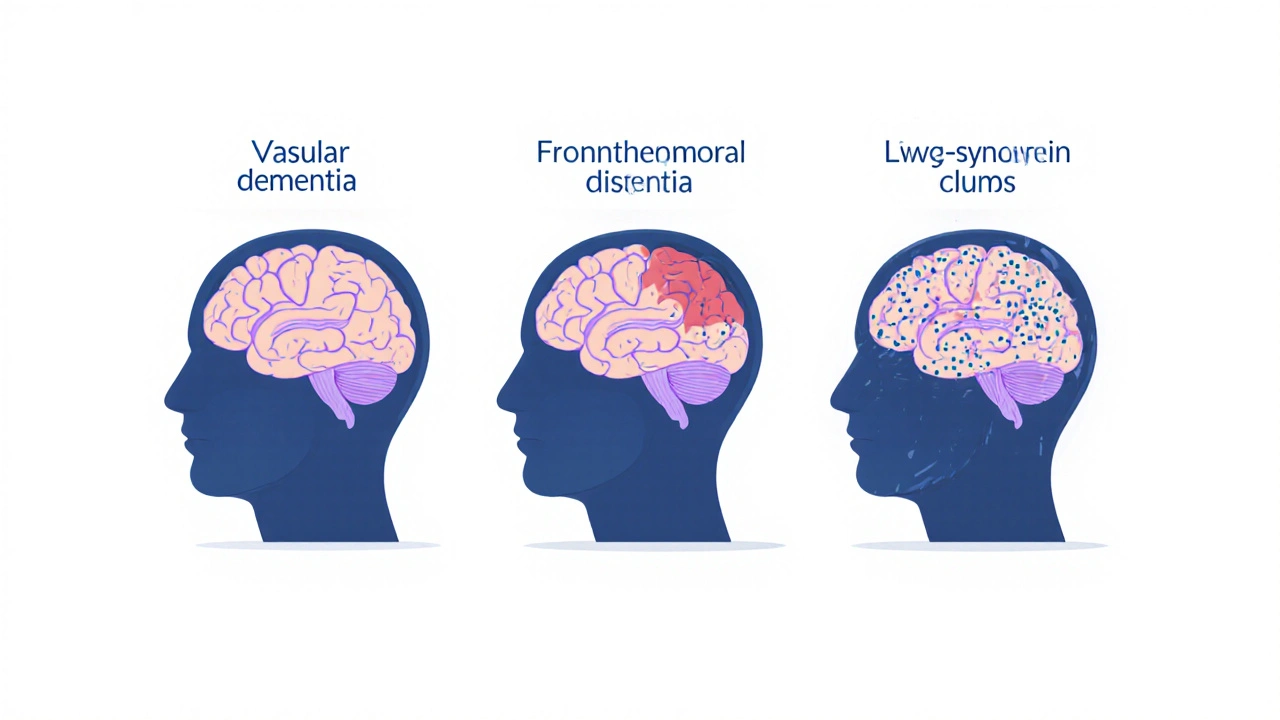
What Makes These Three Dementias Different?
When people talk about dementia, they often mean Alzheimer’s disease. But Alzheimer’s isn’t the only kind. In fact, three other types - vascular dementia, frontotemporal dementia (FTD), and Lewy body dementia (LBD) - are just as common, and just as serious. Each one attacks the brain in a different way, causes different symptoms, and needs a different approach to care. Getting the diagnosis right isn’t just about labels - it’s about avoiding dangerous mistakes. Some medications used for Alzheimer’s can make LBD symptoms worse, even deadly. Misdiagnosing FTD as depression or bipolar disorder delays real help. And ignoring vascular dementia means missing a chance to stop further brain damage.
Vascular Dementia: The Silent Damage From Blood Flow Problems
Vascular dementia happens when blood flow to the brain gets blocked or reduced. This isn’t one single event - it’s often the result of years of high blood pressure, diabetes, or clogged arteries. Small strokes, or mini-strokes called TIAs, build up over time. Each one kills a little bit of brain tissue. The result? Cognitive decline that doesn’t creep in slowly. It jumps. One month, the person seems okay. The next, after a stroke, they can’t remember names, follow instructions, or manage bills.
Unlike Alzheimer’s, where memory fades first, vascular dementia often hits planning, decision-making, and movement first. People may struggle to walk steadily, lose bladder control, or have trouble coordinating simple tasks. Hallucinations and delusions show up more often than in early Alzheimer’s. The brain scans tell the story: white spots, scars, and dead tissue from old clots or bleeds. MRI is the gold standard for spotting this damage.
The good news? You can slow it down. Controlling blood pressure (keeping it under 130/80) cuts dementia risk by up to 20%. Managing blood sugar, lowering cholesterol with statins, and taking daily aspirin (if your doctor says so) can prevent more damage. Lifestyle changes matter - quitting smoking, walking daily, eating less salt. This isn’t just about treating dementia. It’s about preventing more strokes. The SPRINT-MIND trial showed that intensive blood pressure control reduced mild cognitive decline by 19% over five years.
Frontotemporal Dementia: When Personality Changes Before Memory Fades
Frontotemporal dementia hits people young. Most are between 45 and 65 - still working, raising kids, driving. That’s why it’s often mistaken for a midlife crisis, depression, or even schizophrenia. A once-kind, thoughtful person becomes rude, impulsive, or emotionally flat. They might eat non-food items, spend money recklessly, or lose all sense of social rules. Others become silent, repeating the same phrase, unable to find words, even though they can still recognize their own children.
This isn’t memory loss. It’s brain shrinkage in the front and sides - the areas that control behavior, judgment, and language. Pathologists find abnormal clumps of tau or TDP-43 proteins in these regions. Brain scans show clear atrophy. Memory stays strong early on, which is why families are confused. "Why can she remember my birthday but not know how to pay a bill?"
There’s no drug to stop FTD. But symptoms can be managed. SSRIs can help with compulsive behaviors or emotional outbursts. Speech therapy helps with language loss. The hardest part? Getting the diagnosis. Up to half of FTD cases are initially called psychiatric disorders. A neuropsychological test that checks planning and social reasoning - not just recall - is key. And imaging. If the frontal lobe looks thin on an MRI, and behavior changed first, FTD is likely.

Lewy Body Dementia: The Triple Threat of Fluctuations, Hallucinations, and Stiffness
Lewy body dementia is the most misunderstood type. It’s not Alzheimer’s. It’s not Parkinson’s. It’s both. And it’s deadly if treated wrong. The cause? Tiny clumps of a protein called alpha-synuclein - Lewy bodies - that build up in brain areas controlling thinking, movement, and sleep. These clumps disrupt communication between nerve cells.
Three things scream LBD: fluctuating attention (one hour they’re alert, the next they’re zoning out), visual hallucinations (seeing people or animals that aren’t there), and Parkinson’s-like movement (stiffness, slow steps, shaky hands). Many also have REM sleep behavior disorder - acting out dreams, kicking, yelling in their sleep. This often starts years before dementia.
Memory isn’t the first problem. It’s focus. Someone with LBD might describe a detailed scene from a dream, then forget what they ate for breakfast. They might be confused one minute and perfectly clear the next. That’s why doctors miss it. Up to 75% are first diagnosed as Alzheimer’s. But here’s the danger: giving them antipsychotics like haloperidol or even risperidone can cause severe reactions - extreme stiffness, high fever, even death. That’s why cholinesterase inhibitors like rivastigmine are preferred. They help with thinking and hallucinations without the risk.
Dopamine scans (DaTscan) help confirm the diagnosis. They show reduced dopamine activity - a hallmark of Lewy body disease. Survival is usually 5 to 8 years after diagnosis. But with the right care - avoiding dangerous meds, managing sleep, using gentle movement therapy - hospital stays drop by 30%.
How They Compare: Side by Side
| Feature | Vascular Dementia | Frontotemporal Dementia (FTD) | Lewy Body Dementia (LBD) |
|---|---|---|---|
| Primary Cause | Blocked or reduced blood flow to brain | Build-up of tau or TDP-43 proteins in frontal/temporal lobes | Alpha-synuclein clumps (Lewy bodies) in brainstem and cortex |
| Typical Age of Onset | 65+ | 45-65 (most common dementia under 60) | 50+ |
| Early Symptoms | Step-wise decline after stroke, trouble planning, movement issues | Personality changes, poor judgment, language loss - memory often intact | Fluctuating attention, visual hallucinations, Parkinson’s stiffness |
| Memory Loss | Later stage | Minimal early on | Less prominent early than in Alzheimer’s |
| Brain Scan Findings | Infarcts, white matter lesions, strokes visible on MRI | Shrinkage in frontal and temporal lobes | Reduced dopamine uptake on DaTscan; Lewy bodies not visible on standard scans |
| Key Treatment Focus | Control blood pressure, diabetes, cholesterol; prevent strokes | SSRIs for behavior; speech therapy; no disease-modifying drugs | Cholinesterase inhibitors (rivastigmine); avoid antipsychotics |
| Biggest Risk of Misdiagnosis | Attributed to normal aging | Diagnosed as depression, bipolar, or schizophrenia | Diagnosed as Alzheimer’s - leading to dangerous drug use |
Why Getting the Diagnosis Right Matters
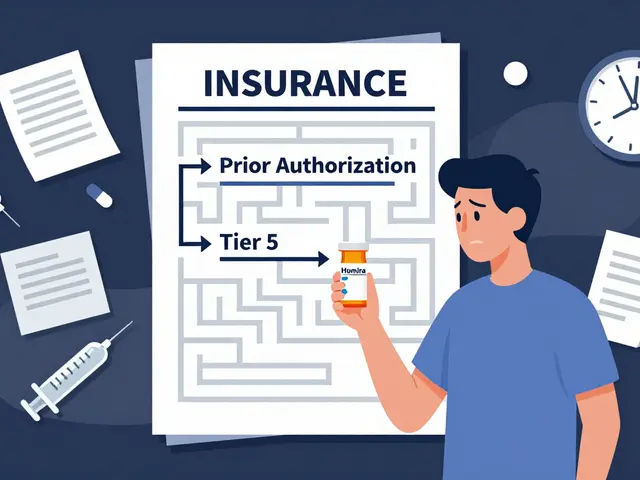
Wrong diagnosis isn’t just a mistake. It’s dangerous. Someone with LBD given an antipsychotic for hallucinations can go into neuroleptic malignant syndrome - a life-threatening reaction with high fever, muscle rigidity, and organ failure. That’s why doctors need to know: is this Alzheimer’s? Or is it LBD?
FTD gets mistaken for mental illness because the behavior changes are so dramatic. A man who starts yelling at strangers or stealing from stores isn’t "going crazy." He’s losing control of his frontal lobe. Treating him with antidepressants might help a little, but it won’t fix the root problem. He needs behavioral support, not just pills.
Vascular dementia is the only one where you can actually prevent more damage. If you catch high blood pressure early, control it, and manage diabetes, you’re not just treating dementia - you’re stopping it. That’s the power of prevention.
And yet, research funding is wildly out of balance. Alzheimer’s gets billions. LBD and FTD together get less than $50 million a year in the U.S., despite affecting millions. That’s why awareness matters. The more people understand these types, the faster they’ll get the right care.
What Comes Next? Hope on the Horizon
There’s no cure yet - but progress is happening. Blood tests are being developed to detect early signs of vascular injury and protein buildup. For LBD, drugs like prasinezumab are being tested to clear alpha-synuclein. For FTD, gene-targeting therapies are in trials for those with inherited forms. And the 2023 Lancet Commission found that controlling just nine risk factors - especially high blood pressure in midlife - could prevent 40% of all dementia cases.
What you can do now: Learn the signs. If a loved one suddenly changes personality, has unexplained hallucinations, or declines after a stroke, push for a specialist. Ask for an MRI. Ask about DaTscan if movement problems are present. Don’t accept "it’s just aging." And if a doctor suggests an antipsychotic for hallucinations in someone over 50 - ask if Lewy body dementia has been ruled out.
Can vascular dementia be reversed?
No, brain damage from strokes can’t be undone. But you can stop it from getting worse. Controlling blood pressure, diabetes, and cholesterol prevents new strokes. Many people stabilize after a few events and live for years with careful management.
Is frontotemporal dementia inherited?
About 10-30% of FTD cases have a strong family history, often linked to mutations in genes like C9orf72, MAPT, or GRN. Genetic testing is available for families with multiple affected members. But most cases are sporadic - no known family link.
Why do people with Lewy body dementia have visual hallucinations?
Lewy bodies disrupt brain areas that process vision and distinguish reality from imagination. These hallucinations are often detailed - seeing children, animals, or strangers - and the person may not realize they’re not real. Unlike in psychosis, they’re usually not frightening to the person. Telling them "it’s not real" often causes distress. Gentle redirection works better.
Can a person have more than one type of dementia?
Yes. Up to 40% of people with Alzheimer’s also have Lewy bodies. Many older adults have both vascular damage and Alzheimer’s changes. This is called mixed dementia. Symptoms may be more severe or progress faster. Diagnosis gets harder, but treatment still focuses on managing all contributing factors.
How long do people live after being diagnosed?
Life expectancy varies. Vascular dementia: 5-10 years after diagnosis, depending on stroke risk. FTD: 6-10 years. LBD: 5-8 years. But many factors affect this - age at diagnosis, overall health, access to care, and whether complications like pneumonia or falls occur. Good symptom management can extend quality life.
What to Do If You Suspect Dementia
If you notice sudden changes in behavior, memory, movement, or thinking in someone over 45, don’t wait. See a neurologist or geriatric specialist. Bring a list of symptoms, when they started, and any recent health events - like a stroke or fall. Ask for:
- A brain MRI to check for strokes or shrinkage
- A DaTscan if movement problems or hallucinations are present
- A neuropsychological test that checks executive function, not just memory
- A review of all medications - especially antipsychotics or sedatives
Write down what you see. People with dementia often don’t realize they’ve changed. You’re the eyes. And your observations could be the key to a correct diagnosis - and the right treatment.





Wow, this post literally saved my grandma’s life. We thought she had Alzheimer’s until her neurologist spotted the white matter lesions on her MRI. Turns out it was vascular dementia-now her BP is under control and she’s walking again. I wish we’d known this sooner.
The distinction between vascular dementia and Alzheimer’s is critically important from a clinical standpoint. The SPRINT-MIND trial data, which demonstrates a 19% reduction in mild cognitive decline with intensive blood pressure management, provides robust, evidence-based justification for early intervention. Furthermore, the avoidance of antipsychotics in Lewy body dementia is not merely a recommendation-it is a life-saving imperative.
Let’s be real-doctors are lazy. They see an older person forgetting names and say ‘Alzheimer’s’ without even looking at a scan. I watched my uncle get prescribed risperidone for ‘hallucinations’-he ended up in the hospital with rigidity and a fever. Turns out it was LBD. The doctor didn’t even know what a DaTscan was. If this post saves one person from getting poisoned by antipsychotics, it’s worth it.
Why is this even a thing? People are dying because doctors don’t know their job. And don’t even get me started on how FTD gets labeled as ‘midlife crisis’ or ‘bad parenting.’ My cousin was diagnosed with bipolar after screaming at a cashier for no reason-turns out his frontal lobe was melting. And now he’s on SSRIs like it’s a mood ring. The system is broken. And yes, I’m mad.
It’s fascinating how cultural perceptions of aging influence diagnostic patterns. In many Western societies, cognitive decline is normalized as ‘just getting old,’ whereas in some East Asian cultures, behavioral changes in elders are more immediately scrutinized. This disparity may contribute to underdiagnosis of FTD and LBD in regions where medical systems prioritize age-based assumptions over neurological evaluation.
Oh great. Another post telling me what I already know. Meanwhile, my mom’s neurologist still doesn’t know the difference between tau and TDP-43. But sure, let’s all feel smart reading this while the actual doctors keep messing up. Congrats on the 10th article on this topic this month.
I’m a caregiver for my mother with FTD. She doesn’t remember my name anymore, but she still laughs at my dumb jokes. This post got me crying-not because it’s sad, but because it finally explained what’s happening. No one ever told me that her impulsivity wasn’t ‘being difficult’-it was her brain. Thank you for writing this.
There’s hope. Seriously. Blood tests for early protein markers are coming. I know a guy whose dad got into a gene therapy trial for FTD-no cure yet, but his speech improved. And for LBD? Prasinezumab could be a game-changer. Don’t give up. Keep pushing for scans, keep asking questions. You’re not just fighting for a diagnosis-you’re fighting for dignity.
Look, I’ve spent 12 years as a paramedic, and I’ve seen it all-people confused after strokes, grandmas talking to dead relatives, guys who used to be CEOs now crying because they can’t button their shirts. This post? It’s the one I wish I’d had when I started. I’ve handed out printed copies to every new EMT trainee since I read it. Knowledge is power, and this is the kind of power that saves lives. Keep doing this work.
It’s ironic that we’ve spent decades pathologizing dementia while ignoring the societal collapse that accelerates it: isolation, poor nutrition, chronic stress, and the commodification of elder care. The real epidemic isn’t alpha-synuclein-it’s capitalism’s abandonment of the aging. We treat brains like machines, then wonder why they break. Fix the system, not just the synapses.
So… what’s the takeaway? Don’t let your grandpa watch TV too much?