Many people think herbal supplements are safe because they’re natural. But that’s a dangerous assumption. If you’re taking prescription drugs-whether it’s blood thinners, antidepressants, or high blood pressure meds-some herbal products can mess with how they work. Not just a little. Sometimes, they can cause bleeding, organ rejection, or even death.
Why This Matters More Than You Think
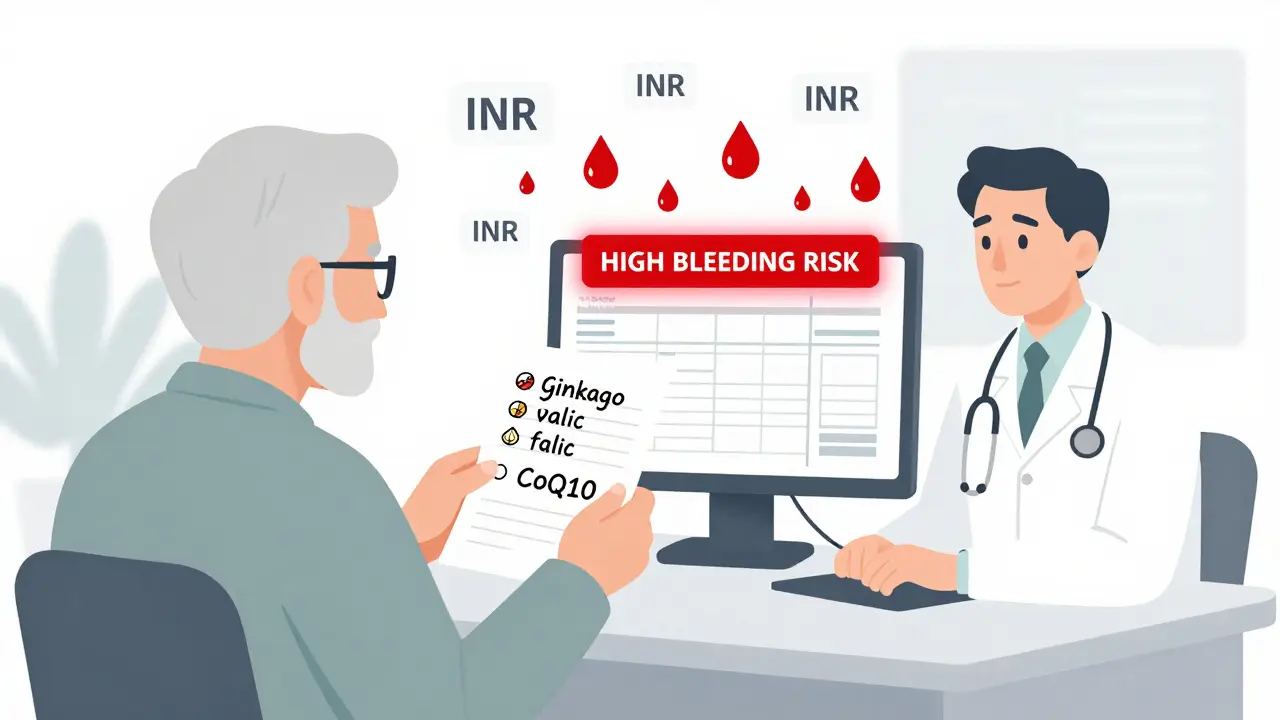
About half of all U.S. adults take at least one herbal supplement. For people over 65, that number jumps to nearly 70%. And here’s the problem: only about one in four of them tells their doctor. That means doctors are flying blind. They prescribe warfarin for a blood clot, but don’t know you’re taking ginkgo biloba every day. The result? Your INR spikes. You start bleeding internally. And no one saw it coming. This isn’t theoretical. Between 2010 and 2020, the Mayo Clinic recorded 23 major bleeding events linked to ginkgo and warfarin-three of them fatal. St. John’s Wort can drop cyclosporine levels by 60%. That’s enough to trigger organ rejection in transplant patients. Garlic supplements slash saquinavir, an HIV drug, by over half. And cranberry juice? It’s hit or miss-sometimes it boosts warfarin’s effect, sometimes it doesn’t. No one knows why.The Top 5 Dangerous Herbal Supplements
Not all herbs are risky. But these five have clear, documented, life-threatening interactions with common prescriptions.- St. John’s Wort: This is the most dangerous herb on the list. It turns off enzymes in your liver that break down drugs. That means your meds get flushed out too fast. It reduces antidepressants like sertraline by 20-40%, cuts oral contraceptives by 15-30%, and can make HIV drugs like saquinavir useless. One study found 78% of users on Drugs.com reported birth control failure. That’s not a glitch. That’s a pattern.
- Ginkgo biloba: Used for memory and focus, but it thins your blood. When combined with warfarin, aspirin, or apixaban, it increases bleeding risk by 300%. One Reddit user, u/HeartPatient99, ended up in the ER with an INR of 8.2 after mixing ginkgo with apixaban. He had severe rectal bleeding. His doctors said this happens more than people realize.
- Garlic supplements: Garlic in food is fine. Garlic pills? Not so much. They reduce the effectiveness of saquinavir by 51%. They also boost the effect of blood thinners. In a 2019 trial with 18 healthy volunteers, garlic dropped saquinavir levels to dangerous lows. If you’re on HIV meds, skip the garlic capsules.
- Goldenseal: This herb blocks CYP3A4, a key liver enzyme. That means drugs like midazolam, statins, and even some cancer treatments don’t break down properly. A 2018 study showed a 40% drop in midazolam clearance. That can lead to overdose symptoms-drowsiness, slow breathing, even coma.
- Coenzyme Q10: Often taken for heart health or energy, CoQ10 can weaken warfarin’s effect. Mayo Clinic’s 2022 analysis showed a 25-30% drop in anticoagulant activity. If you’re on warfarin and start taking CoQ10, your INR could drop. That means clots. That means stroke. You need weekly INR checks when starting or stopping this combo.
What About the Others?
Some herbs are lower risk-but still not harmless.- Ginseng: Can raise or lower blood pressure unpredictably. With calcium channel blockers, it might drop your BP too far. With MAO inhibitors (used for depression), it can trigger serotonin syndrome-high fever, muscle stiffness, confusion. That’s an emergency.
- Hawthorn: Used for heart health, but it can cause your blood pressure to crash when mixed with beta-blockers like metoprolol. One case report showed systolic pressure dropping to 80 mmHg in a patient on both.
- Licorice: It acts like a diuretic. If you’re on furosemide or hydrochlorothiazide, it can drain your potassium. That leads to muscle cramps, irregular heartbeat, even cardiac arrest.
- Chamomile: Mild blood-thinning effect. Not as bad as ginkgo, but if you’re on warfarin or have surgery coming up, skip it.
On the other hand, black cohosh, milk thistle, saw palmetto, and American ginseng have minimal documented interactions. That doesn’t mean they’re 100% safe-but they’re far less likely to cause harm.
How to Protect Yourself
You don’t have to quit supplements. But you need to be smart.- Make a list. Write down every pill, powder, tea, or tincture you take-even if you think it’s harmless. Include brands and doses.
- Bring it to every appointment. Don’t wait for your doctor to ask. Say, “Here’s what I’m taking.”
- Check your labels. Many “brain health” supplements contain ginkgo. “Mood support” often has St. John’s Wort. “Immune boosters” usually include garlic. You might be taking them without knowing.
- Watch for warning signs. If you’re on warfarin and start bleeding easily, bruising more, or your INR jumps above 4.0, stop the supplement and call your doctor. If you’re on antidepressants and feel agitated, feverish, or your muscles lock up, that’s serotonin syndrome. Go to the ER.
- Use the NCCIH Herb-Drug Interaction Checker. It’s free, updated quarterly, and ranks interactions from “life-threatening” to “moderate.” Bookmark it.
Why the System Is Broken
The Dietary Supplement Health and Education Act (DSHEA) of 1994 lets companies sell herbal products without proving they’re safe. The FDA can only act after someone gets hurt. That’s why 17 companies got warning letters in 2022 for secretly adding actual drugs-like sildenafil or steroids-into “natural” supplements. Only 15% of herb-drug interactions have strong clinical proof. Most are based on case reports or lab studies. That’s why doctors are hesitant to warn patients. But the evidence is piling up. In 2023, the FDA received over 4,000 reports of supplement-related harm. Experts estimate 95% of cases go unreported. And 18% of emergency visits from supplements in adults over 65 involve herb-drug interactions.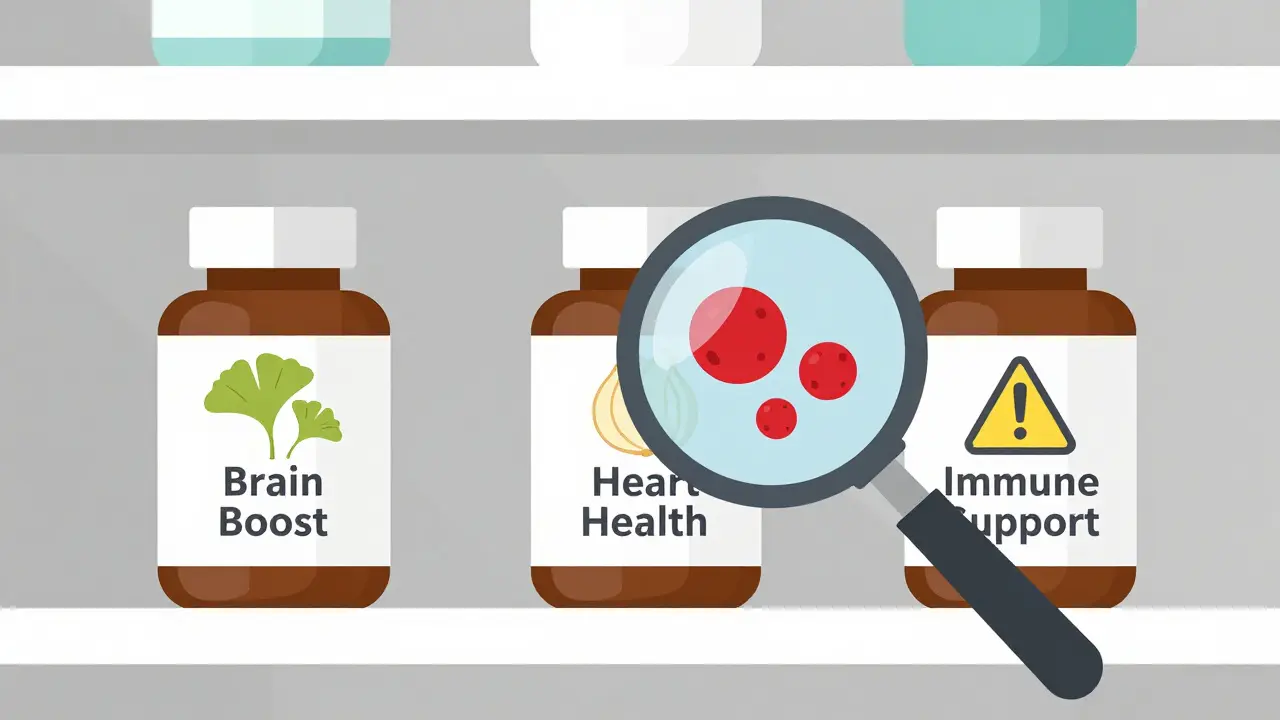
What’s Changing
The good news? Things are starting to shift. Epic Systems, the biggest electronic health record provider, plans to integrate the NCCIH interaction database into its medication reconciliation tools by Q3 2025. That means when your doctor prescribes a new drug, the system might pop up: “Warning: Patient takes St. John’s Wort. Risk of reduced antidepressant efficacy.” The European Medicines Agency already has a standardized risk rating system. The U.S. is catching up. But until then, you’re your own best defense.Final Word: Natural Doesn’t Mean Safe
Herbal supplements aren’t evil. Many people benefit from them. But they’re powerful. They change how your body processes medicine. And if you’re on prescriptions, that’s not a gamble you can afford to take. Don’t assume your pharmacist knows what you’re taking. Don’t assume your doctor will ask. Don’t assume “natural” means harmless. If you’re taking any prescription drug-especially blood thinners, antidepressants, HIV meds, or transplant drugs-talk to your doctor before taking anything herbal. Bring your bottles. Ask: “Could this interfere with my medication?” It’s not paranoia. It’s protection.Can herbal supplements really make my prescription drugs stop working?
Yes. St. John’s Wort can reduce the levels of antidepressants, birth control pills, and HIV drugs by up to 80%. Ginkgo biloba can make blood thinners like warfarin too strong, causing dangerous bleeding. Garlic supplements can cut the effectiveness of HIV medications like saquinavir by more than half. These aren’t rare side effects-they’re well-documented in clinical studies.
Is it safe to take ginkgo biloba if I’m on aspirin?
No. Ginkgo biloba has blood-thinning properties. When combined with aspirin, warfarin, or other anticoagulants, it significantly increases your risk of bleeding. Studies show a 300% higher risk of hemorrhage compared to aspirin alone. Even if you’re only taking low-dose aspirin daily, combining it with ginkgo can lead to internal bleeding, stroke, or death.
Why don’t doctors always warn patients about herbal interactions?
Many doctors don’t ask because they assume patients won’t tell them. Only 25% of people who take herbal supplements mention it to their provider. Plus, the evidence isn’t always clear-cut-some interactions are based on case reports, not large trials. But that doesn’t mean they’re not real. The risk is high enough that experts like the Mayo Clinic and American Academy of Family Physicians now recommend routine screening.
Are all herbal supplements regulated like prescription drugs?
No. Under U.S. law (DSHEA), herbal supplements don’t need FDA approval before being sold. Companies don’t have to prove they’re safe or effective. The FDA can only act after harm occurs. That’s why you’ll find supplements with hidden drugs-like sildenafil or steroids-in products labeled “natural.” There’s no guarantee of quality or safety.
What should I do if I think an herbal supplement is affecting my medication?
Stop taking the supplement immediately and contact your doctor or pharmacist. If you’re on warfarin and notice unusual bruising, nosebleeds, or dark stools, get an INR test right away. If you’re on antidepressants and feel feverish, confused, or your muscles are rigid, go to the ER-these are signs of serotonin syndrome, which can be fatal. Don’t wait. Document what you took, when, and what symptoms you’re having.
Can I take cranberry juice with warfarin?
It’s unpredictable. Some studies show cranberry juice can raise INR levels, increasing bleeding risk. Others show no effect. The difference may come from the amount consumed, your genetics, or other medications. Because the risk isn’t clear, most experts recommend avoiding large amounts of cranberry juice or supplements if you’re on warfarin. If you drink it regularly, get your INR checked more often.
Is there a reliable source to check for herb-drug interactions?
Yes. The National Center for Complementary and Integrative Health (NCCIH) offers a free, updated Herb-Drug Interaction Checker. It classifies interactions as life-threatening, significant, or moderate. Memorial Sloan Kettering Cancer Center also maintains a detailed database. Both are backed by clinical data and updated quarterly. Avoid random websites or supplement company claims-stick to these trusted sources.






This is so important!! 🙏 I just started my mom on ginkgo for 'memory' and had no idea it could mess with her blood thinner. I'm taking her to the pharmacy tomorrow to get it checked. Thank you for this!
Natural doesn't mean safe. Period.
Okay but like... if the FDA doesn't regulate it, why are we even talking about this? Someone's gonna sell you a 'miracle herb' that's just sugar and chalk anyway. 🤷♀️
The author presents this as if every herbal supplement is a ticking time bomb. This is alarmist nonsense. People have taken St. John’s Wort for decades without incident. The real issue is poor medical communication, not the supplements themselves. The fear-mongering here is worse than the interactions.
I appreciate the data, but I'm still skeptical. If these interactions are so dangerous, why aren't there more public health campaigns? Why do pharmacies still sell these without warning labels? This feels like a selective scare tactic.
I’m a nurse, and I’ve seen this firsthand. A patient on warfarin took ginkgo for ‘brain fog’ and ended up with a GI bleed. She didn’t think it mattered because it was ‘natural.’ She didn’t even know ginkgo was an herb. This isn’t theoretical. It’s daily. If you’re on meds, list everything-even that ‘chill’ tea you drink before bed.
so like... st. john's wort makes birth control fail?? no wonder my cousin got preggo on 'natural mood boosters' lmao. also why is garlic bad but garlic bread is fine?? is it the capsule? or is this just big pharma fearmongering? 🤔
I’ve been on warfarin for 12 years... I stopped cranberry juice cold turkey after reading this. And honestly? My INR’s been more stable since. I used to think it was just coincidence. Now I know better. Also-why does no one talk about how some supplements are just sugar pills with a fancy label? I bought one labeled 'Heart Support' and the ingredients list was: 'proprietary blend.' That’s not a supplement. That’s a trap.
This is such a needed post!! 🌿❤️ I told my grandma to stop her garlic pills after her cardiologist mentioned it. She cried because she thought they were helping her 'clean her blood.' Now she’s on a simple regimen and feels better than ever. Thank you for the clarity.
I think this is really well-researched. I’ve had patients come in with INR levels off the charts and no idea why. It’s always something they picked up online. I just wish more people would bring their supplement bottles to appointments. It’s not about judgment-it’s about safety.
As someone who works in global health, I find this particularly alarming in low-resource settings. Many patients self-medicate with herbal remedies because pharmaceuticals are unaffordable or inaccessible. Without provider education or standardized labeling, these interactions become deadly. We need international guidelines-not just U.S.-centric warnings.
It’s funny how we’ll take a pill with 17 chemicals and call it medicine, but a plant-based extract is 'dangerous' because it's 'natural.' The truth is, chemistry doesn’t care about origin. What matters is dose, interaction, and context. Maybe the real problem is that we treat 'natural' like a moral virtue instead of a biochemical variable.
The sheer negligence in this space is criminal. Companies market ginkgo as 'cognitive support' while burying the interaction warnings in 8-point font. The FDA’s inaction is not oversight-it’s abandonment. And doctors? They’re too busy to ask. Patients are left to gamble with their lives on Amazon reviews. This isn’t healthcare. It’s a horror show.
I'm tired of people acting like supplements are some kind of moral high ground. You take them because you're scared of real medicine. You think 'natural' means 'better' and now you're bleeding out because you didn't tell your doctor you were popping ginkgo pills like candy. Wake up.
The data presented here is accurate, but the framing is misleading. Many of these interactions are dose-dependent and occur only with high-dose extracts. Consuming garlic in food is not equivalent to taking 1,000 mg capsules daily. The distinction matters. This post conflates culinary use with pharmacological dosing, which unnecessarily frightens people.