When you need a life-saving drug like HIV antiretrovirals or cancer treatment, the price shouldn’t depend on where you live. But it does. Thanks to the TRIPS agreement, the cost of generic medicines in poor countries has been locked in by international patent rules that favor big drug companies over patients. This isn’t theoretical-it’s why millions in Africa, Asia, and Latin America still wait months or years to get affordable drugs that exist, but are blocked by legal barriers.
What the TRIPS Agreement Actually Does
The TRIPS agreement, created in 1994 under the World Trade Organization, forced every member country to adopt the same minimum rules for patenting drugs. Before TRIPS, many developing countries didn’t even allow product patents on medicines. They could copy how a drug was made (process patents) and produce their own versions. That’s how India became the pharmacy of the developing world-making cheap generics for HIV, malaria, and hepatitis C. TRIPS changed that. It required all 164 WTO members to grant 20-year product patents on medicines, starting from the filing date. That meant countries like South Africa, Brazil, and Thailand could no longer legally make or import cheaper versions of patented drugs-even if people were dying without them. The idea was simple: protect innovation. But in practice, it protected profits.How Patents Block Generic Drugs
Patents aren’t the only barrier. Even after a drug’s patent expires, companies use other tricks to delay generics. One is data exclusivity. When a company runs clinical trials to get a drug approved, they submit all that data to health regulators. TRIPS doesn’t require data exclusivity, but many countries added it anyway. That means generic makers can’t use that data to prove their version works. They have to run their own expensive trials. Result? A 5-10 year delay in generic entry, even after the patent ends. Then there’s patent linkage. Some countries now require health agencies to check if a drug is still under patent before approving a generic. That gives patent holders a direct line to block generics without going to court. The Access to Medicine Foundation found that 65% of low-income countries now use this system-far beyond what TRIPS requires.Compulsory Licensing: The Loophole That Almost Didn’t Work
TRIPS does allow governments to override patents in emergencies. This is called compulsory licensing. A country can say: “We need this drug now. We’re not waiting.” They can let a local company make it, even if the patent holder says no. But here’s the catch: the original TRIPS rule said these licenses had to be used “predominantly for the domestic market.” So if you’re a small country like Rwanda or Botswana and don’t have a drug factory, you’re out of luck. You can’t import generics made in India under a compulsory license-even if India is willing to make them. That changed in 2005, with a “Paragraph 6 Solution.” It let countries without manufacturing capacity import generics made under compulsory license from others. Sounds fair, right? But the paperwork was a nightmare. Countries had to prove they couldn’t make the drug themselves, issue a license, notify the patent holder, and track every pill. By 2016, only one shipment of malaria medicine had ever moved under this rule.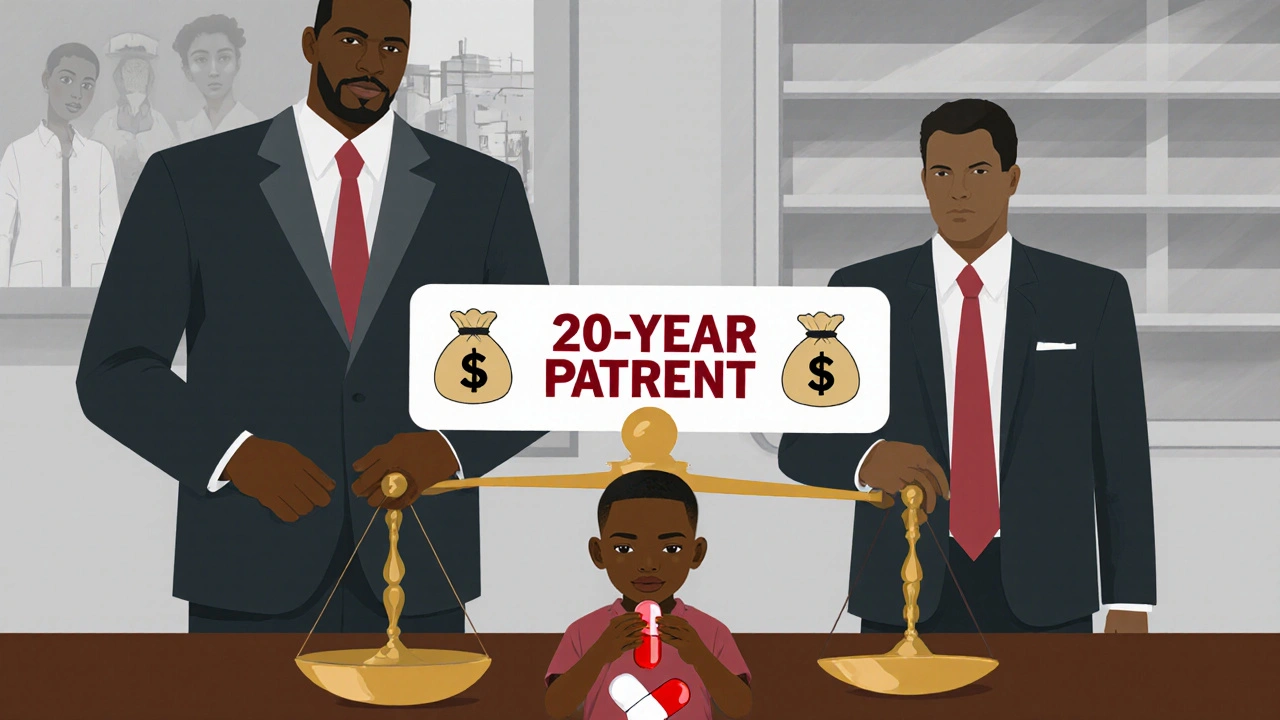
Real-World Consequences: When Laws Cost Lives
In 1998, South Africa passed a law to let public hospitals import or make cheaper HIV drugs. Forty pharmaceutical companies sued. They claimed it violated TRIPS. The world watched as a country fighting an AIDS epidemic was threatened with legal action for trying to save lives. Public pressure forced the companies to drop the case in 2001. Brazil took a different path. In 2000, it started making its own generic antiretrovirals. The U.S. threatened trade sanctions under Section 301. Brazil didn’t back down. The U.S. eventually withdrew the threat. Brazil now provides free HIV treatment to over 400,000 people-mostly thanks to generics. India’s transition to TRIPS-compliant patent laws in 2005 caused a 300-500% spike in cancer drug prices. A drug that cost $1,000 a month jumped to $5,000. Patients died waiting. Only later did Indian courts start rejecting weak patents-like one on the leukemia drug imatinib-allowing generics to return.TRIPS Plus: The Hidden Rules That Make Things Worse
TRIPS is the floor, not the ceiling. Wealthy countries like the U.S. and EU push “TRIPS Plus” terms in free trade deals. These add extra protections beyond what TRIPS requires:- Patent term extensions-adding years to the 20-year patent
- 8-10 years of data exclusivity (TRIPS allows none)
- Blocking generic approval even if the patent is invalid
- Restricting compulsory licensing to only extreme emergencies
The COVID-19 Waiver: A Glimmer of Change
In October 2020, India and South Africa asked the WTO to temporarily waive TRIPS rules for vaccines, tests, and treatments during the pandemic. Over 100 countries supported it. The U.S., EU, and Switzerland blocked it for over a year. In June 2022, they agreed to a limited waiver-only for vaccines, only for low- and middle-income countries, only for a few years. It was a win, but a weak one. It didn’t cover treatments or diagnostics. It didn’t remove data exclusivity. And it didn’t apply to countries that still produce vaccines, like South Africa. Still, it was the first time the WTO had ever modified TRIPS for public health.





TRIPS is just corporate welfare dressed up as law. I get that pharma needs to make money, but when people die because a pill costs 10x more in their country, that’s not innovation-that’s exploitation. And the fact that countries like India were the pharmacy of the world before TRIPS proves we didn’t need this system to begin with.
This is one of the most important public health discussions of our time. The moral failure here isn’t just in policy-it’s in our collective silence. We celebrate breakthroughs in medicine while ignoring who gets to benefit from them. The data is clear: patents aren’t the barrier to innovation-they’re the barrier to equity.
Oh please. If we let every country ignore patents, we’ll have no new drugs in 10 years. People forget that drug development costs billions. Someone has to pay for it. If you want cheap drugs, stop blaming the companies and start blaming your government for not funding healthcare properly.
Let’s cut through the noise: TRIPS is a regulatory capture masterpiece. Big Pharma lobbied for 20-year monopolies, then pushed TRIPS-plus clauses into every trade deal like a cartel. Data exclusivity? Patent linkage? These aren’t ‘protections’-they’re anti-competitive maneuvers disguised as IP law. The WHO’s own data shows 80% of medicines are off-patent yet still inaccessible. That’s not a market failure-it’s a theft.
And don’t even get me started on the COVID waiver. A 2-year, vaccine-only, paperwork-heavy loophole that took 18 months to negotiate? That’s not compromise. That’s performative cruelty. We had the tools. We had the will. We just chose profit over people.
Meanwhile, the NIH funded 70% of the foundational science behind modern antivirals and mRNA tech. Taxpayers paid for the breakthroughs. Corporations priced the cures. That’s not capitalism. That’s feudalism with a patent office.
The Medicines Patent Pool is the only real solution here. Voluntary licensing, not litigation. Collaboration, not coercion. And if countries like Kenya and Ethiopia build local manufacturing? That’s not just access-it’s sovereignty.
Bottom line: If your life depends on a pill, your zip code shouldn’t be your death sentence. TRIPS was never about science. It was about control.
While the humanitarian implications of the TRIPS agreement are indeed profound, it is imperative to recognize the structural incentives that underpin pharmaceutical innovation. Without robust intellectual property protections, the capital-intensive nature of drug development would be disincentivized, potentially leading to a stagnation in therapeutic advancement. The balance between access and innovation remains delicate, and any recalibration must be undertaken with rigorous economic and ethical consideration.
India's generic industry is a miracle, but it's built on the backs of Western R&D. Why should we reward countries that copy instead of create? 🤔💊
I think what’s often missing in these conversations is the human cost behind the statistics. A mother in Uganda waiting six months for her child’s HIV meds isn’t debating IP law-she’s praying. A man in Brazil choosing between rent and his cancer pills isn’t analyzing trade agreements-he’s surviving. The real question isn’t whether patents should exist, but whether we can afford to let profit decide who lives and who dies.
TRIPS isn’t the problem-it’s the enforcement. Countries that signed it had the option to use flexibilities like compulsory licensing, but they didn’t. They caved to pressure from the U.S. and EU. That’s not a flaw in the agreement-it’s a failure of leadership. We need governments with spine, not just activists screaming into the void.
So we should let poor countries steal from American companies? Next you’ll say we should give away iPhones for free because some people can’t afford them. Wake up.
This is just another leftist rant wrapped in a ‘human rights’ bow. The market works. If you want cheap drugs, move to a country that doesn’t have a broken healthcare system. Stop blaming the innovators.
When I was a kid in rural India, my uncle got his TB meds from a local pharmacy for $2 a month. After 2005, the same drug cost $150. My uncle died waiting. TRIPS didn’t protect innovation-it protected greed. We didn’t lose patents. We lost our dignity.
why do we even have patents if the science is all public funded anyway?? like come on
TRIPS is a tool of neocolonialism. The West imposed it. The Global South paid the price. No innovation without equity. End of story.
If you remove intellectual property rights, what’s to stop China from copying every drug and flooding the market? Who will fund the next breakthrough if no one can profit? This isn’t about morality-it’s about sustainability.
It’s ironic that the same people who argue for open access to knowledge in software and education resist it in medicine. If knowledge is meant to be shared, why is a molecule treated differently than a line of code?