Secondary Hypogonadism & Metabolic Syndrome Risk Calculator
Metabolic Syndrome: Presence of 3+ of these 5 criteria:
- Waist circumference ≥ 94 cm (men)
- Fasting glucose ≥ 100 mg/dL
- Triglycerides ≥ 150 mg/dL
- HDL cholesterol < 40 mg/dL
- Blood pressure ≥ 130/85 mmHg
Secondary Hypogonadism: Testosterone level < 300 ng/dL with low LH/FSH
Note: This tool provides a general risk estimate based on common clinical indicators. For accurate diagnosis, consult a healthcare professional.
Metabolic Syndrome Risk
Secondary Hypogonadism Risk
Key Findings
Recommendations
Ever wondered why men with low testosterone often also struggle with blood‑sugar spikes, belly fat, or high blood pressure? The answer lies in the two‑way street between secondary hypogonadism and metabolic syndrome. Understanding this connection helps doctors spot hidden risks and gives patients clear steps to turn the tide.
What Is Secondary Hypogonadism?
Secondary hypogonadism is a condition where the testes produce insufficient testosterone because the brain’s signaling glands-namely the pituitary and hypothalamus-fail to release enough luteinizing hormone (LH) and follicle‑stimulating hormone (FSH). Unlike primary hypogonadism, the testes themselves are structurally normal; the problem starts upstream. Common triggers include pituitary tumors, chronic opioid use, severe stress, and systemic illnesses that depress the hypothalamic‑pituitary‑gonadal (HPG) axis.
What Is Metabolic Syndrome?
Metabolic syndrome is a cluster of inter‑related risk factors-abdominal obesity, elevated fasting glucose, high triglycerides, low HDL‑cholesterol, and hypertension-that together raise the odds of type2 diabetes and cardiovascular disease. The syndrome reflects chronic insulin resistance and low‑grade inflammation, often rooted in lifestyle, genetics, and aging.
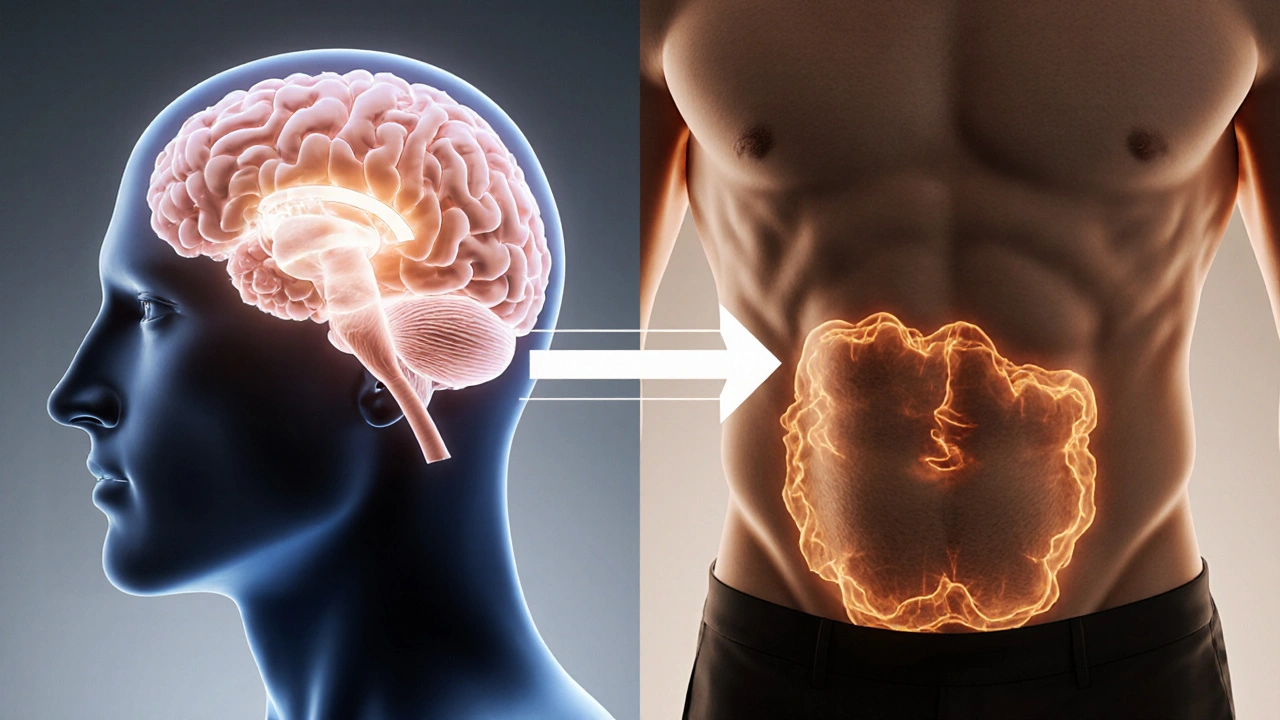
Why the Two Conditions Overlap
Several biological bridges tie secondary hypogonadism to metabolic syndrome:
- Insulin resistance dampens LH release. High insulin levels interfere with hypothalamic GnRH pulses, leading to lower LH and FSH output.
- Low testosterone drives visceral fat accumulation. Testosterone normally blocks adipocyte expansion in the abdomen; without it, fat cells grow larger and secrete more inflammatory cytokines.
- Inflammatory cytokines (IL‑6, TNF‑α) impair gonadal steroidogenesis, creating a feedback loop that deepens both hormone deficiency and metabolic dysfunction.
- Shared risk factors-obesity, chronic stress, certain medications-can trigger both conditions simultaneously.
In short, a drop in testosterone can seed metabolic derangements, and those derangements can pull the HPG axis further down.
Key Clinical Evidence
Large cohort studies from the UK and the US have shown:
- Men with diagnosed secondary hypogonadism have a 2-3× higher prevalence of metabolic syndrome compared with age‑matched controls.
- Each 10nmol/L (≈300ng/dL) decline in serum testosterone raises the odds of developing insulin resistance by about 15%.
- Intervention trials where testosterone replacement therapy (TRT) was added to lifestyle changes reported modest reductions in waist circumference (average−3cm) and fasting glucose (average−0.4mmol/L) over 12months.
These data underscore a bidirectional relationship rather than a one‑way cause‑effect story.
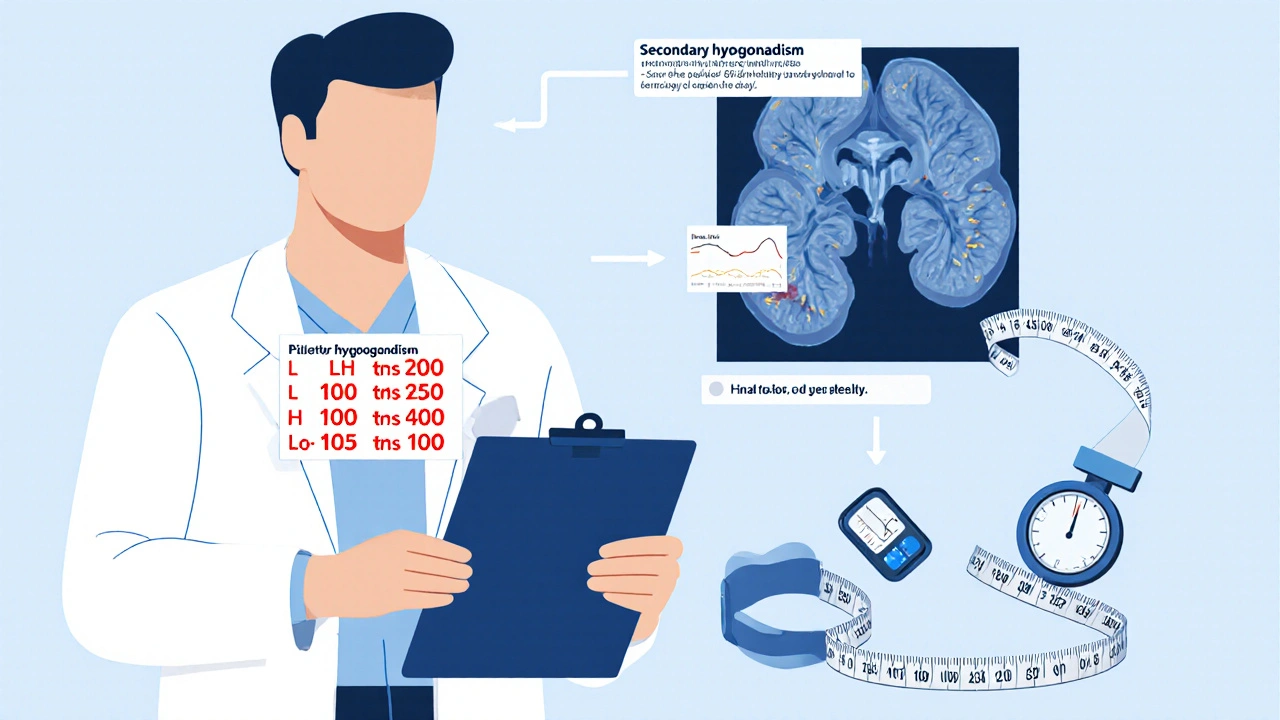
Diagnosing Overlap: What to Look For
When a patient presents with one condition, clinicians should screen for the other:
- Secondary hypogonadism work‑up: morning total testosterone, LH, FSH, prolactin, and a pituitary MRI if LH/FSH are low.
- Metabolic syndrome assessment: waist circumference, fasting glucose, lipid panel, and blood pressure measured on two separate visits.
- Calculate the HOMA‑IR index (fasting insulin×glucose/22.5) to gauge insulin resistance; values>2.5 suggest a high‑risk profile.
Linking the labs often reveals a pattern: low testosterone + low LH/FSH + elevated HOMA‑IR + high triglycerides.
Management Strategies That Hit Both Targets
Because the conditions reinforce each other, a combined approach works best.
Lifestyle First
- Weight loss: a 5-10% reduction in body weight can lift testosterone levels by 10-20% and improve insulin sensitivity.
- Resistance training: strength workouts boost muscle mass, which directly stimulates LH secretion.
- Sleep hygiene: 7-9hours of uninterrupted sleep normalizes nocturnal testosterone spikes.
- Stress reduction: mindfulness or CBT lowers cortisol, which otherwise suppresses GnRH.
Medical Interventions
- Testosterone Replacement Therapy (TRT): indicated when symptoms align and testosterone < 300ng/dL with low LH/FSH. Benefits include improved insulin sensitivity, reduced waist circumference, and better lipid profiles. Monitoring includes PSA, hematocrit, and periodic lipid checks.
- Insulin‑sensitizing agents: Metformin or GLP‑1 receptor agonists can lower HOMA‑IR and may indirectly assist testosterone recovery.
- Address pituitary causes: If a tumor or medication is the root, treat that first-surgery, dose adjustment, or alternative analgesics.
Follow‑Up Checklist
- Re‑measure testosterone, LH, and FSH every 3months after initiating TRT.
- Track waist circumference and fasting glucose quarterly.
- Adjust lifestyle plan based on weight change; aim for ≤90cm waist for men.
- Screen for cardiovascular events annually (ECG, lipid panel).
Quick Reference Table
| Feature | Secondary Hypogonadism | Metabolic Syndrome | Overlap Area |
|---|---|---|---|
| Primary Hormone | Low testosterone (testosterone < 300ng/dL) | Normal‑range testosterone may be present | Low testosterone often co‑exists with insulin resistance |
| LH/FSH Levels | Low or inappropriately normal | Usually normal | Insulin resistance can blunt LH secretion |
| Waist Circumference | May be elevated due to fat gain | ≥94cm (men) is a diagnostic criterion | Visceral fat drives both conditions |
| Fasting Glucose | Often normal unless diabetes present | ≥100mg/dL (5.6mmol/L) is a criterion | Low testosterone aggravates hepatic glucose output |
| Blood Pressure | Can be normal or elevated | ≥130/85mmHg | Androgen deficiency contributes to vascular stiffness |
Practical Takeaways for Patients and Clinicians
- Screen men with metabolic syndrome for secondary hypogonadism-especially if they have fatigue, low libido, or reduced muscle mass.
- When secondary hypogonadism is confirmed, evaluate lifestyle factors first; weight loss alone can correct mild hormone deficits.
- TRT is a useful adjunct but should not replace core metabolic interventions like diet, exercise, and glucose‑lowering meds.
- Regular monitoring of both endocrine and metabolic markers prevents missed complications.
Frequently Asked Questions
Can metabolic syndrome cause secondary hypogonadism, or is it the other way around?
Both directions are true. Chronic insulin resistance and high inflammatory cytokines can suppress LH release, leading to secondary hypogonadism. Conversely, low testosterone promotes visceral fat and insulin resistance, deepening metabolic syndrome.
What lab values confirm secondary hypogonadism?
A morning total testosterone below 300ng/dL (≈10nmol/L) paired with low or inappropriately normal LH (<5IU/L) and FSH suggests secondary hypogonadism. Free testosterone, SHBG, and pituitary imaging may be added for confirmation.
Is testosterone replacement therapy safe for men with heart disease?
Current evidence indicates that TRT, when monitored, does not increase major cardiovascular events in men with stable disease. However, patients with recent myocardial infarction or uncontrolled hypertension should defer TRT until their condition stabilizes.
How quickly can lifestyle changes raise testosterone levels?
Weight loss of 5-10% typically lifts total testosterone by 10-20% within 3-6months. Adding resistance training can amplify this rise by another 5-10%.
Should all men with low testosterone be tested for metabolic syndrome?
Yes. Because the two conditions frequently coexist, a full metabolic work‑up (waist, glucose, lipids, blood pressure) is recommended whenever hypogonadism is diagnosed.




Yo, this whole hype about testosterone being the magic fix is straight-up BS. The government’s health guidelines are just a smokescreen, and anyone who buys into this nonsense is buying a ticket to a broken system. Get real, folks.
Great point! It's super important to remember that lifestyle changes can make a huge difference. Even small steps like walking daily or swapping sugary drinks for water can shift the whole picture.
The interrelationship between secondary hypogonadism and metabolic syndrome warrants rigorous clinical scrutiny. Evidence suggests a bidirectional causality mediated by insulin resistance and inflammatory cytokines.
Exactly, and patients need a clear action plan. Start with a structured diet and progressive resistance training; those are non‑negotiable pillars for reversing both conditions.
Reading through this article, I couldn't help but notice the sloppy phrasing scattered throughout-'low testosterone level detected' versus 'testosterone level < 300ng/dL', for instance. Such imprecision does a disservice to clinicians who rely on precise thresholds. Moreover, the authors gloss over the fact that not all men with hypogonadism will develop metabolic syndrome; epidemiological nuance is essential. The omission of randomized controlled trial data is a glaring weakness, and the reliance on observational cohorts introduces bias. In short, the piece reads like a rushed literature summary rather than a rigorous synthesis.
While your pedantic concerns are noted, the core message remains unchanged: low testosterone correlates with adverse metabolic profiles, and that fact is well‑documented across multiple meta‑analyses.
🤝 Hey everyone, I just wanted to take a moment to celebrate how this discussion bridges science and personal empowerment. It's fascinating how a hormone as old as testosterone can still surprise us with its modern health implications. First, the link between visceral fat and androgen deficiency is not merely correlative; it's mechanistic, involving leptin resistance and chronic inflammation. Second, lifestyle interventions-especially consistent strength training-act as a natural testosterone booster, which in turn can dampen insulin resistance. Third, dietary patterns rich in omega‑3 fatty acids and low in refined sugars have been shown to improve both lipid profiles and hormonal balance. Fourth, adequate sleep, typically seven to nine hours, restores the nocturnal surge of testosterone that many of us miss due to shift work or screen addiction. Fifth, stress management techniques such as mindfulness or even a simple walk in nature can lower cortisol, a hormone that antagonizes testosterone production. Sixth, it's crucial for healthcare providers to screen men presenting with metabolic syndrome for secondary hypogonadism, because the treatment cascade can differ dramatically. Seventh, when testosterone replacement is considered, it must be paired with vigilant monitoring of hematocrit, PSA, and cardiovascular risk factors. Eighth, the emerging class of GLP‑1 receptor agonists not only improves glycemic control but may also have a favorable impact on weight, indirectly supporting hormonal health. Ninth, community support groups provide accountability and shared experiences, which dramatically increase adherence to lifestyle changes. Tenth, the stigma around men discussing hormonal health is fading, and that cultural shift is a victory in itself. Eleventh, let’s not forget the role of vitamin D and zinc as co‑factors in steroidogenesis; supplementation may be beneficial when deficiencies are identified. Twelfth, regular follow‑up every three months ensures that any therapeutic adjustments are timely and evidence‑based. Thirteenth, patient education materials should be clear, avoiding medical jargon that can alienate the very individuals we aim to help. Fourteenth, interdisciplinary collaboration between endocrinologists, dietitians, and physical therapists yields the most comprehensive outcomes. Finally, remember that each small, sustainable habit compounds over months into significant health gains. Keep pushing, stay informed, and celebrate every win-even the tiny ones! 😊
That’s solid advice dudes
Ah, the age‑old dance of hormones and metabolism-like two clumsy partners at a never‑ending gala. One could argue that the body is just trying to keep us humble, reminding us that we aren’t the masters of our own chemistry. Yet, with a dash of discipline and a sprinkle of modern medicine, we can at least learn the steps. So, if your testosterone decides to take an early vacation, perhaps it’s the universe nudging you toward greener pastures-namely, better lifestyle choices.
Exactly, it’s all about finding that rhythm that works for each individual. Encouraging small, consistent changes can turn the tide, and the data backs up that approach. Let’s keep sharing resources and stories so others feel less alone on this journey.
Reading through the presented material, one cannot help but appreciate the thoroughness with which the authors have delineated the diagnostic criteria for both secondary hypogonadism and metabolic syndrome; however, it would be advantageous to incorporate a clearer algorithmic flowchart, thereby facilitating clinicians' decision‑making processes. Additionally, explicit mention of follow‑up intervals-perhaps at three‑month and six‑month milestones-could enhance patient management strategies. In sum, the article is commendable, yet these refinements would render it indispensable.