When your doctor orders a brain MRI, it’s not just a scan-it’s a window into what’s happening inside your brain. Unlike X-rays or CT scans, MRI doesn’t use radiation. Instead, it uses powerful magnets and radio waves to create detailed pictures of brain tissue. This makes it the most trusted tool for spotting problems like strokes, tumors, multiple sclerosis, and even early signs of dementia. But what do those images actually show? And how do doctors tell the difference between normal aging and something serious?
What Brain MRI Actually Shows
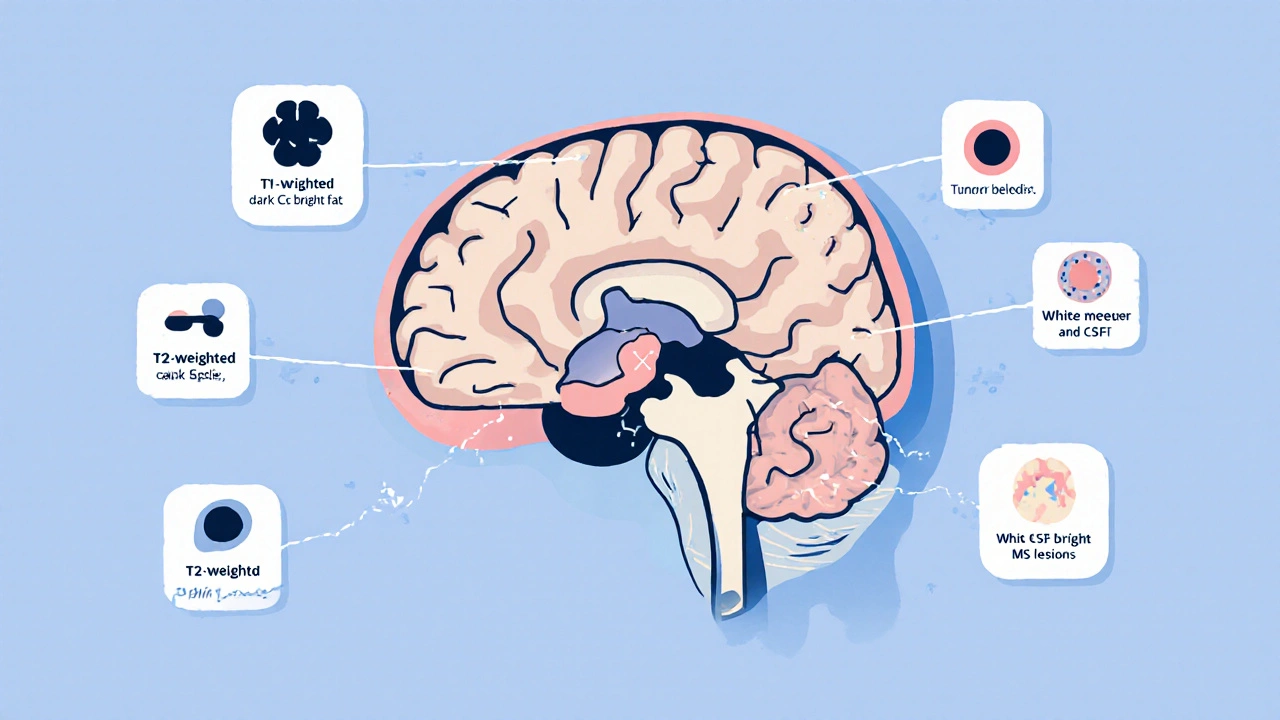
A brain MRI doesn’t just give you a picture-it gives you multiple pictures, each highlighting different things. These are called sequences, and each one tells a different story. The three most important ones are T1-weighted, T2-weighted, and FLAIR.
T1-weighted images are like a high-resolution anatomy map. Fat and certain types of tissue show up bright white. Cerebrospinal fluid (CSF), which fills the spaces around your brain, looks dark. This sequence is great for seeing the shape of your brain, the size of your ventricles, and whether there’s any swelling or mass pushing things out of place.
T2-weighted images flip the script. Water becomes bright. That means anything with extra fluid-like swelling from an injury, infection, or inflammation-lights up like a beacon. But here’s the catch: CSF also looks bright on T2. That’s why it can be tricky. A dark spot on T1 might be a bleed. A bright spot on T2 might be a tumor. Or it might just be normal fluid.
That’s where FLAIR comes in. FLAIR stands for Fluid-Attenuated Inversion Recovery. It’s a special version of T2 that turns CSF dark again, while keeping abnormal fluid (like lesions from multiple sclerosis) bright. This is critical. Without FLAIR, you might mistake normal fluid-filled spaces for disease. With it, you can clearly see those telltale white spots around the ventricles that signal MS.
Common Findings and What They Mean
Not every bright spot is a disaster. Many findings are normal-or at least common with age. Here are the most frequent things radiologists see and what they mean.
White matter hyperintensities-those small bright spots on T2 and FLAIR-are seen in nearly 90% of people over 70. They’re often linked to tiny blood vessel changes from high blood pressure or aging. They’re called leukoaraiosis in medical terms. While they don’t always cause symptoms, they do raise the risk of stroke and cognitive decline over time.
Lacunar infarcts are tiny strokes, usually less than 5mm, that happen deep in the brain-often in the basal ganglia or thalamus. They’re caused by blockages in small arteries. You might not feel them. Many people live with them without knowing. But if you have several, it’s a sign your brain’s small vessels are under stress.
Multiple sclerosis plaques look different. They’re often oval, located near the ventricles, and run perpendicular to the brain’s surface. They’re called Dawson’s fingers. Unlike age-related spots, they tend to appear in multiple areas and change over time. FLAIR makes them stand out. If you’re under 50 and have these, MS is a real possibility.
Acute stroke shows up fast on a special sequence called DWI (diffusion-weighted imaging). Within minutes of a stroke, water movement in brain cells gets restricted. DWI picks this up immediately. That’s why MRI is now the gold standard for stroke diagnosis. CT can miss early strokes-MRI doesn’t.
Tumors can be tricky. Some look like swelling. Others enhance with contrast dye. A meningioma, for example, often hugs the skull and lights up brightly after contrast. A glioma might spread into brain tissue without a clear border. Size, location, and how it reacts to contrast help doctors tell them apart.
Microbleeds are tiny leaks from fragile blood vessels. They show up as dark dots on SWI (susceptibility-weighted imaging) or gradient echo sequences. They’re common in older adults with high blood pressure or amyloid angiopathy. Finding more than five can raise concern for future bleeding risk.
Why MRI Beats CT for Neurological Problems
CT scans are fast. They’re great for trauma-like a head injury after a fall. But when it comes to neurological conditions, CT is like looking at a blurry photo. MRI is like zooming in with a 4K lens.
Here’s why:
- CT can’t see small lesions in the brainstem or cerebellum well. Bone blocks the view. MRI sees right through it.
- CT misses early strokes. MRI catches them in under 30 minutes.
- CT can’t distinguish between old and new MS plaques. MRI can.
- CT exposes you to radiation. MRI doesn’t. That’s why it’s preferred for kids and for people who need repeated scans.
But MRI isn’t perfect. It takes longer-30 to 45 minutes. You have to lie still. It’s noisy. And if you have a pacemaker, certain metal implants, or severe claustrophobia, you might not be able to have one. In emergencies, CT still wins because speed saves lives.
What MRI Can’t Tell You
Even with all its power, MRI doesn’t give you the full picture. A bright spot on FLAIR doesn’t tell you if it’s causing symptoms. It doesn’t tell you if it’s getting worse. It doesn’t tell you if it’s related to your headaches or memory lapses.
That’s why doctors don’t just look at images. They combine MRI findings with your symptoms, your medical history, and sometimes other tests-like spinal fluid analysis or blood work.
For example, a 45-year-old with headaches and a single small white matter lesion? Probably nothing. But if that same person has numbness in their legs, vision changes, and bladder issues? That changes everything.
And here’s something most people don’t realize: MRI finds incidental findings in up to 10% of scans done for headaches with no neurological signs. Most are harmless-like a tiny cyst or an old silent stroke. But they can cause anxiety, extra tests, and even unnecessary treatments. That’s why the American College of Radiology says MRI isn’t usually needed for simple migraines without warning signs.
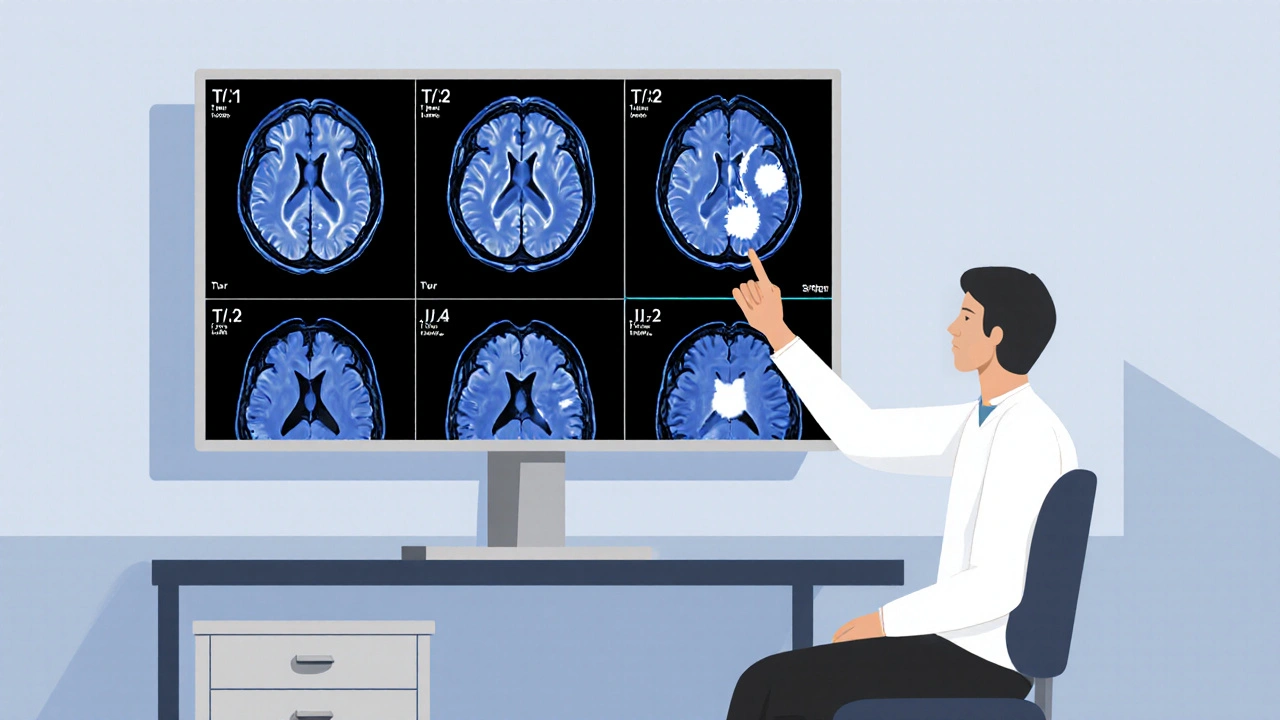
How Radiologists Read a Brain MRI
Reading a brain MRI isn’t random. It’s a step-by-step process.
First, they check the midline. Is the brain centered? Is the third ventricle too wide? That could mean pressure or atrophy.
Then they look at the ventricles. Are they enlarged? That might be normal aging-or early dementia.
Next, they move to the deep structures: thalamus, basal ganglia, brainstem. Are there small bright spots? That’s where lacunar strokes hide.
Then the lobes: frontal, parietal, temporal, occipital. Are there abnormal signals? Is one side swollen? Temporal lobe lesions could mean herpes encephalitis. Parietal-occipital changes might point to posterior reversible encephalopathy syndrome (PRES), often linked to high blood pressure or pregnancy.
Finally, they check the cerebellopontine angle-the space between the cerebellum and brainstem. That’s where small tumors like vestibular schwannomas hide. They’re rare, but MRI catches them as small as 2mm. Miss them on CT? Almost guaranteed.
And they always compare sequences. A lesion that’s bright on T2 and FLAIR but dark on T1? Likely fluid-filled. Bright on T1 too? Could be fat, blood, or contrast dye.
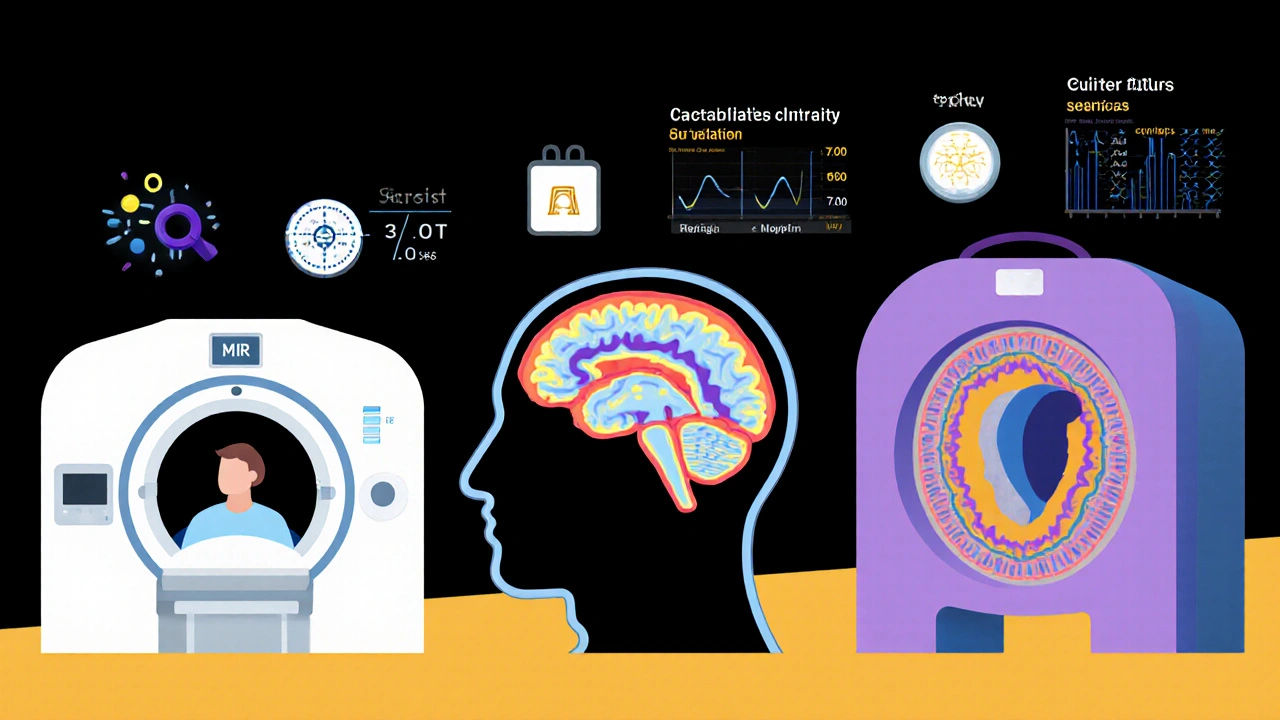
What’s New in Brain MRI
Technology is moving fast. While most hospitals use 1.5T or 3.0T machines, some academic centers now have 7.0T scanners. These show brain layers so clearly, you can see individual cortical bands. It’s still research-only-but it’s changing how we understand brain diseases.
Artificial intelligence is helping too. New software can cut scan time in half without losing detail. It can automatically detect MS plaques, measure brain volume changes over time, and even predict which patients are at higher risk of dementia based on subtle patterns.
Quantitative MRI is another big leap. Instead of just saying “there’s a lesion,” it measures things like water content, blood flow, or myelin levels. These numbers can track disease progression more accurately than just looking at pictures.
And while MRI is still expensive-ranging from $1,200 to $3,500 in the U.S.-it’s becoming more accessible. In South Africa, public hospitals are slowly upgrading, and private clinics are offering more affordable packages. Still, access remains uneven, especially in rural areas.
What You Should Know Before Your Scan
If you’re scheduled for a brain MRI, here’s what matters:
- You’ll need to remove all metal-jewelry, piercings, even some makeup with metallic particles.
- Let them know if you have implants, pacemakers, or metal fragments (especially from old injuries).
- It’s loud. You’ll get earplugs or headphones.
- You have to lie still. Even a little movement blurs the images.
- Contrast dye isn’t always needed. It’s only used if the doctor suspects a tumor, infection, or inflammation.
- The scan takes 30-45 minutes. Bring something to help you relax.
And remember: a brain MRI doesn’t give you a diagnosis. It gives you clues. Your doctor puts those clues together with everything else to make sense of them.
Can a brain MRI show anxiety or depression?
No, a brain MRI cannot directly show anxiety or depression. These are functional and chemical conditions, not structural ones. While research has found subtle differences in brain volume or activity patterns in people with long-term depression, these aren’t visible enough to diagnose the condition. MRI is used to rule out physical causes-like tumors or strokes-that could mimic mental health symptoms.
Why do I need contrast dye for some brain MRIs?
Contrast dye (usually gadolinium) helps highlight areas where the blood-brain barrier is broken. This happens in tumors, infections, or active inflammation like MS flare-ups. Normal brain tissue blocks the dye. If the dye leaks in, it means something abnormal is happening. It doesn’t mean cancer-it just means something is disrupting the barrier.
Are brain MRI results always accurate?
MRI is highly accurate for detecting structural changes, but interpretation matters. A bright spot could be a stroke, a tumor, or just an old injury. Radiologists use multiple sequences and clinical context to tell the difference. Mistakes happen-especially when images are blurry, or when the patient moves. That’s why a second opinion is sometimes recommended for unclear findings.
Can MRI detect early Alzheimer’s disease?
Yes, MRI can show signs that suggest early Alzheimer’s, like shrinkage in the hippocampus-the memory center of the brain. But it can’t confirm the diagnosis on its own. Alzheimer’s is defined by the presence of amyloid plaques and tau tangles, which MRI can’t see. Special PET scans or spinal fluid tests are needed for confirmation. Still, MRI helps track progression and rule out other causes like tumors or normal pressure hydrocephalus.
Is it safe to have multiple brain MRIs over time?
Yes, it’s safe. MRI doesn’t use radiation, so repeated scans don’t carry the same risks as CT or X-rays. The only concern is repeated use of gadolinium contrast, which can rarely deposit in the brain. For most people, this isn’t harmful, but doctors avoid contrast unless necessary. If you need frequent monitoring-like for MS or a brain tumor-your doctor will weigh the benefits against any potential risks.





Bro this is the most clear breakdown of MRI sequences I've ever seen 😍 T1, T2, FLAIR like a superhero trio saving brains from misdiagnosis. I used to think radiologists just guessed. Now I know they're decoding brain hieroglyphics. 🧠✨
This is why America leads in medical tech. Other countries are still using X-rays like it's 1985. We have 7T scanners that can see your neuron's morning coffee stain. Don't let the socialists take this away.
In India we don't have access to this tech in 90% of hospitals. But we still diagnose better than you with just a stethoscope and intuition. Your fancy machines just confirm what our doctors already knew. #IndianMedicineWins
I had a brain MRI last year. Found a tiny spot. Doctor said 'probably nothing.' Then I spent three weeks Googling 'early signs of brain tumor' and now I'm convinced I'm dying. Thanks, internet.
The FLAIR sequence is a critical diagnostic modality in neuroimaging protocols, and its fluid-attenuated inversion recovery properties are indispensable for lesion detection, particularly in demyelinating pathologies such as multiple sclerosis, where CSF suppression enhances lesion conspicuity. Also, the 3.0T field strength remains the clinical gold standard. Period.
I'm from the Midwest and I had no idea MRI could be so beautiful. It's like seeing the inside of a galaxy. I used to think my brain was just a mushy lump. Now I see it as this intricate, delicate masterpiece. I cried when I saw my own scan. Not because I was scared. Because it was so... alive.
They don't tell you the truth. The contrast dye? It's laced with nanobots. They're mapping your brain for the next phase of the global surveillance program. That's why they say it's 'safe.' They want you to think it's safe. Look up 'gadolinium deposition' and tell me that's not a cover-up.
We treat the scan like it's truth but it's just a shadow of what's happening. The real diagnosis is in the silence between the patient's words. The tremor in their hand. The way they avoid eye contact. The MRI shows a lesion. But only the human being can tell you if it's hurting them.
I'm a neuro nurse and I've seen this play out a hundred times. Someone gets a white spot on their MRI, panics, Googles 'brain tumor survival rate,' and shows up at the ER with a printed 17-page article. Then we explain it's just age-related small vessel disease. They cry. We hug. Then they go home and thank us. This post? It's the kind of thing that could save someone from a mental breakdown.
I had a brain MRI after my 'mysterious headaches' and they found NOTHING. But then I saw the radiologist's notes: 'incidental finding: tiny arachnoid cyst.' I spent 2 months researching it. Turns out it's harmless. But now I'm convinced my brain is secretly holding a secret society meeting in there. And they're judging me.
They say MRI is safe. But what about the EMF? What about the magnets pulling out your dental fillings? What if they're using it to implant chips? I heard they do this in California. I'm not paranoid. I'm prepared.
I'm a marketing director and I just saw a 7T MRI demo at a conference. It's wild. You can see the individual folds in the cortex like a fingerprint. We're gonna make a viral TikTok series called 'What Your Brain Looks Like When You're High.' Probably gonna go viral. Also, I'm hiring a neuroscientist to consult. DM me.
You people are so naive. This whole post is corporate propaganda. The MRI industry makes billions. They push these scans because they're profitable, not because they're necessary. That 'incidental finding' you're so scared of? It's a money trap. They find something vague, then bill you for five more tests. You're not being helped. You're being monetized.
i think the part about white matter hyperintensities being common after 70 is super important. i had one on my scan and i thought i was gonna die but now i feel better. also i think the part about how ct misses early strokes is like... yeah i know but like why do we still use ct? like if mri is better why not just do it all the time? maybe its the cost or something idk. anyway thanks for this
Lemmy, you're right about CT vs MRI. But here's the real issue: insurance companies won't pay for MRI unless you're bleeding from the ears. So doctors have to use CT first. It's not about tech. It's about $$$. P.S. Your typo-prone typing is oddly endearing. Keep it real.