Medication Risk Calculator & Decision Aid
Your Personalized Medication Risk Assessment
This tool helps you understand your personalized risk for certain conditions to make better-informed medication decisions. Enter your information below to see your calculated risk and how it affects your treatment options.
Your Risk Assessment
What this means for your medication choices:
What matters most to you?
Benefit: 3.5% lower risk of heart disease
Risk: 1.2% chance of side effects
Benefit: 1.8% lower risk of heart disease
Risk: None
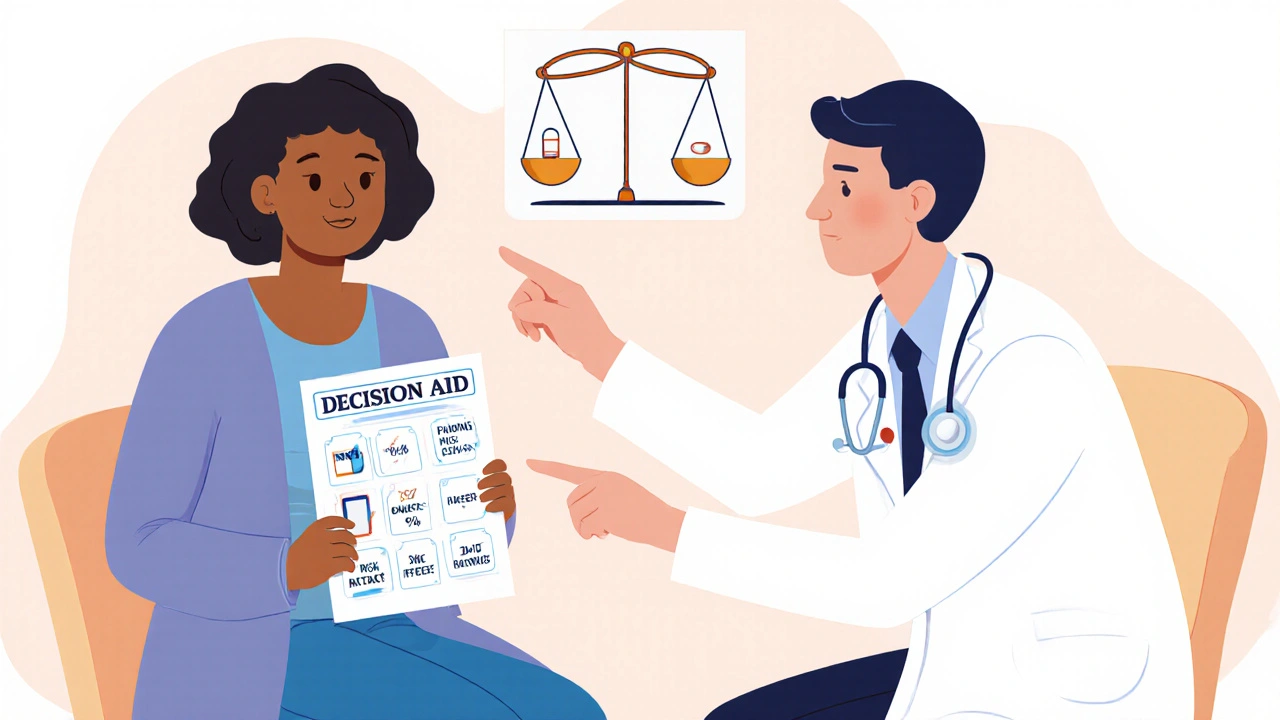
Every year, hundreds of thousands of people in the U.S. are harmed by medication errors. Many of these aren’t caused by doctors or pharmacists making mistakes-they happen because patients don’t fully understand what they’re taking, why, or what the real risks are. That’s where patient decision aids come in. These aren’t fancy apps or complicated tools. They’re simple, evidence-based resources that help people make smarter, more confident choices about their medications. And the data shows they work.
What Are Patient Decision Aids?
Patient decision aids (PDAs) are tools-paper, digital, or video-that give people clear, balanced information about their medication options. They don’t tell you what to do. Instead, they show you the facts: how likely a drug is to help, what side effects you might face, and how your personal values fit into the equation. Think of them as a fairness coach for your healthcare decisions. They’re built around the International Patient Decision Aids Standards (IPDAS), a set of 12 rules that make sure these tools are trustworthy. A good PDA gives you equal info on all options-including choosing not to take any medication. It shows real numbers, not vague warnings like “may cause side effects.” It asks you questions like: “How important is avoiding a heart attack versus avoiding daily pills?” Over 150 validated decision aids exist today, covering conditions like diabetes, high cholesterol, depression, and arthritis. Tools like the “Statin Choice” aid or “Diabetes Medication Choice” help patients see their actual risk numbers-not the scary generalizations they often hear in the clinic.How Do They Improve Medication Safety?
Medication errors happen when people start, stop, or mix drugs without understanding the trade-offs. PDAs fix this by turning confusion into clarity. In one study, patients using a decision aid for statins learned their 10-year risk of heart disease wasn’t “high” as their doctor said-it was 7.2%. That changed their mind. They chose not to start the medication, avoiding unnecessary side effects like muscle pain or liver stress. That’s safety through informed choice. Another study found that patients who used a decision aid before starting insulin for diabetes were 24% more likely to stick with the treatment six months later. Why? Because they understood the benefits and knew what to expect. No surprises. No fear-driven abandonment. The numbers don’t lie:- Patients using PDAs score 13.28 points higher on medication knowledge tests than those who just get verbal advice.
- Decisional conflict-feeling torn, unsure, or anxious-drops by 8.7 points on a standard scale.
- Patients are 43% less likely to stay undecided after using a decision aid.
Real Stories: What Patients Say
On Reddit, a user named u/Type2Journey wrote: “The statin decision aid helped me understand my actual 10-year CVD risk was 7.2%, not the ‘high risk’ my doctor mentioned-this prevented me from starting unnecessary medication with potential side effects.” Another patient, after using a diabetes decision aid, said: “I thought insulin meant I failed. The tool showed me it’s just the next step-like upgrading your phone. I didn’t feel ashamed anymore.” Surveys show 87% of patients say PDAs helped them understand medication trade-offs better. Nearly 8 in 10 say they felt less anxious about their choices. That’s huge. Fear leads to skipping doses. Confusion leads to overdosing. Clarity leads to safety.
What About Doctors? Are They Using These Tools?
Yes-but not everywhere. Adoption has grown from 12% of U.S. primary care doctors using PDAs in 2015 to 37% in 2022. Top adopters are in oncology, cardiology, and endocrinology-the areas where medication choices have the biggest impact. The biggest barrier? Time. A typical decision aid adds 3 to 8 minutes to a visit. In a 15-minute slot, that’s tough. But clinics that solve this see big wins. Some hand out the aid before the visit. Others use it during the wait. One clinic in Michigan lets patients complete the tool on a tablet in the exam room while the doctor preps. Dr. Sarah Chen, a primary care provider, shared: “Using the Diabetes Medication Choice decision aid reduced my patients’ insulin hesitation from 42% to 18% in six months. The first few times took longer-but now it’s part of our routine.” Clinicians who use PDAs also report feeling more confident in their recommendations. They’re not pushing a drug. They’re guiding a choice. That changes the whole dynamic.Who Benefits the Most?
PDAs work best for preference-sensitive decisions-where there’s no single “right” answer. Statins? Yes. Antibiotics for a mild sinus infection? Less so. Emergency meds? Probably not. They’re most effective for:- Chronic conditions (diabetes, high blood pressure, depression)
- Medications with significant side effects (statins, anticoagulants, opioids)
- Options with clear trade-offs (pill vs. injection, generic vs. brand)
How Are These Tools Getting Better?
The field is evolving fast. Newer PDAs are now integrated with electronic health records. They pull your lab results, age, weight, and other meds to give you personalized risk estimates. The NIH is funding a system that uses AI to tailor options based on your real data-not generic averages. In 2022, the FDA started recognizing certain decision aids as part of medication labeling for complex drugs. That means when you read a drug’s package insert, you might also get a link to a validated decision tool. By 2025, CMS plans to require decision aids for 12 new clinical scenarios under Medicare Advantage plans. That’s a huge push. If insurers start paying for them, adoption will explode.
What’s Holding Them Back?
Not the science. The system. Most doctors still get paid per visit, not for good outcomes. Spending 5 extra minutes on a decision aid doesn’t earn them more money. That’s why adoption is slow in fee-for-service settings. Some tools are clunky. Paper versions get lost. Digital ones need internet. Older patients struggle with apps. The best tools are simple, mobile-friendly, and work offline. And yes-some people still feel overwhelmed. Too many numbers. Too many options. That’s why training matters. Clinicians need to know how to guide, not just hand out a tablet.Where to Find Trusted Decision Aids
You don’t need to build one. Use a validated tool. The Ottawa Hospital Research Institute’s Decision Aids Library has over 100 free, IPDAS-certified tools. All are evidence-based, free to use, and available in multiple languages. Other trusted sources include:- AHRQ’s Patient Decision Aids Collection
- The Mayo Clinic Shared Decision-Making Resource Center
- Consumer Reports Health Decision Tools
What’s Next?
By 2027, experts predict 75% of high-stakes medication decisions will involve a validated decision aid. Why? Because the evidence is solid. They reduce errors. They improve adherence. They save money long-term by preventing hospitalizations. The real win? Patients stop feeling like passive recipients of care. They become active partners. And when you understand your meds, you’re less likely to hurt yourself by accident. If you’re taking any medication with unclear benefits or serious side effects, ask your provider: “Is there a decision aid for this?” If they say no, ask why. And if they don’t know what you’re talking about-send them to the Ottawa Library. It’s free. It’s proven. And it might just keep you safe.Are patient decision aids only for people with chronic illnesses?
No. While they’re most commonly used for chronic conditions like diabetes or high cholesterol, they’re helpful anytime there’s a preference-sensitive choice. That includes deciding whether to start an antidepressant, choose between two pain medications, or even whether to take a blood thinner after surgery. If there’s more than one reasonable option and the best choice depends on your personal values, a decision aid can help.
Can patient decision aids replace a doctor’s advice?
No. They’re designed to support, not replace, clinical advice. A decision aid gives you facts and helps you think about what matters to you. But only your doctor can interpret your test results, rule out dangers, and recommend what’s medically appropriate. Think of it like a GPS: it shows you routes, but you still need to drive.
Do I need a smartphone to use a decision aid?
Not at all. While many are digital, paper versions are just as effective-and often preferred by older adults. Many clinics print them out or mail them ahead of appointments. The key isn’t the format-it’s whether the tool follows evidence-based standards like IPDAS. A well-designed paper aid can be just as powerful as an app.
How do I know if a decision aid is trustworthy?
Look for certification from IPDAS or endorsement by major health organizations like AHRQ, Mayo Clinic, or the Cochrane Collaboration. A trustworthy tool will: present balanced options, show real numbers (not just “high risk”), help you clarify your values, and avoid pushing one choice. Avoid tools that are made by drug companies unless they’re independently reviewed.
Will my insurance cover the cost of using a decision aid?
Most decision aids are free to use. The tools themselves don’t cost patients anything. However, some insurance plans, especially Medicare Advantage, now reimburse providers for using them during visits. That means your doctor might be paid for spending extra time walking you through one. If you’re asked to pay for a decision aid, it’s likely not a certified one.



OMG this is so needed 😭 I was scared to start my blood pressure med until I used a decision aid and realized my risk was only 5% higher than average. No more fear-driven pills! 🙌
I’ve seen patients hesitate for weeks over statins because they didn’t understand the numbers. Once they saw their actual 10-year risk on paper, everything clicked. Simple tools like this save so much unnecessary stress.
The evidence presented here is compelling and methodologically sound. Patient decision aids align with principles of shared decision-making, which is a cornerstone of ethical clinical practice. Their integration into routine care is not merely beneficial-it is imperative.
Look, I’ve read every Cochrane review on this, and honestly, most of these 'decision aids' are just glorified pamphlets with pretty charts. Real medicine isn’t about making patients feel good-it’s about making them compliant. You think a 72-year-old grandma with arthritis really cares about 7.2% risk numbers? No. She wants a pill that works. Stop overcomplicating it.
And don’t even get me started on the 'IPDAS certified' nonsense. That’s just bureaucratic jargon for 'we spent a lot of time making a PDF.' The real world runs on trust, not spreadsheets.
Also, the FDA recognizing these? That’s like certifying a Yelp review as medical-grade. The system is broken, and this is just more glitter on a sinking ship.
PS: I’ve worked in three hospitals. Nobody uses these unless forced. And even then, they’re left on the counter. 🤷♂️
So you’re telling me… people are too dumb to listen to their doctor? That’s why we have all these errors? Wow. Just wow. If you can’t follow basic instructions, maybe you shouldn’t be taking meds at all. This feels like coddling.
This is the kind of stuff that actually changes lives. Not flashy tech, not expensive apps-just clear info given with care. I’ve seen patients go from paralyzed by fear to confident in their choices. That’s not just better health-it’s dignity. Let’s push this everywhere.
I didn’t even know these existed until last month. I used one for my antidepressant choice and cried. Not because I was sad-because for the first time, I felt like I had a say. My doctor didn’t push. He just asked, 'What matters most to you?' And that changed everything.
Now I tell everyone. Even my uncle in Florida. He printed the paper version and brought it to his appointment. His PCP was shocked. Said he’d never seen it before.
Why isn’t this standard? Why does it feel like a secret?
Important note: The 13.28-point increase in knowledge scores comes from a meta-analysis of 27 RCTs (Cochrane 2021). The 8.7-point drop in decisional conflict is validated via the 16-item Decisional Conflict Scale. Also, the 43% reduction in indecision was replicated across three U.S. health systems-Mayo, Kaiser, and VA. These aren’t anecdotes-they’re reproducible outcomes.
And yes, time is a barrier, but studies show that when integrated into EHRs, the average time per patient drops to 3.2 minutes after the first three uses. Training matters. Tools must be templated, not custom-built.
Also: Avoid tools that don’t include ‘no treatment’ as an option. That’s a violation of IPDAS Standard #5.
Man, this hits different. Back home in Kerala, my aunt was told she 'must' take insulin. She refused for a year because she thought it meant she was 'broken.' Then someone gave her a simple illustrated aid-showed her how insulin is like refilling a battery, not admitting defeat. She started it. Now she walks 5km every morning. No shame. Just science.
These tools don’t just inform-they heal the stigma. And that’s priceless.
Yeah right. Next they'll make us fill out a form before breathing. Doctors know best. Let them do their job. Stop making patients think. It's exhausting.
Used one for my cholesterol meds. Thought I was high risk. Turns out my numbers were fine-just had bad genetics. Didn’t need a pill. Saved $800 a year. My doctor was cool about it. Didn’t push. Just said, 'Good call.' That’s the vibe we need more of.
There’s something beautiful here-not just in the data, but in the philosophy. Medicine has spent decades treating bodies like machines. But we’re not circuits. We’re humans with fears, values, lives outside the clinic. A decision aid doesn’t just give facts-it gives back agency. And maybe, just maybe, that’s the real cure.
I used the statin tool last year. My doctor didn’t even bring it up. I found it myself on the Ottawa site. Printed it. Brought it in. He was surprised… then really impressed. We spent 10 minutes talking. Best visit I’ve had in years.
PS: Paper works. I’m 68. I don’t do apps.
so like… uhh… doctors get paid more if we take meds right?? 😐 like… is this just a way to make us feel better while they still make money??
Empirical evidence supports the efficacy of validated patient decision aids in reducing decisional conflict and improving medication adherence. Their integration into clinical workflows represents a significant advancement in patient-centered care.