You’re here for a straight answer: does ethambutol belong in latent TB infection (LTBI) treatment? Short truth-almost never. It’s a workhorse in active TB while we wait for drug susceptibility results, but it isn’t part of standard LTBI regimens. There are narrow edge cases in drug-resistant exposure where experts may add it, but even then, it’s not the star. Below is the clear, usable version of why, what to use instead, and what to do when things aren’t textbook.
TL;DR: Ethambutol’s role in LTBI
- Standard LTBI therapy does not include ethambutol. Preferred regimens are rifamycin- and/or isoniazid-based (3HP, 4R, 3HR, 6-9H; in some settings, 1HP).
- Ethambutol is bacteriostatic and mainly used for active TB as a companion drug; it offers little benefit for latent bacilli and adds optic neuritis risk.
- Possible exception: contacts of drug-resistant TB (especially MDR/RR-TB). Even there, WHO and national programs favor levofloxacin-based regimens; ethambutol is rarely added and only under expert guidance.
- If a patient can’t take rifamycins, use isoniazid (6-9 months) rather than swapping in ethambutol.
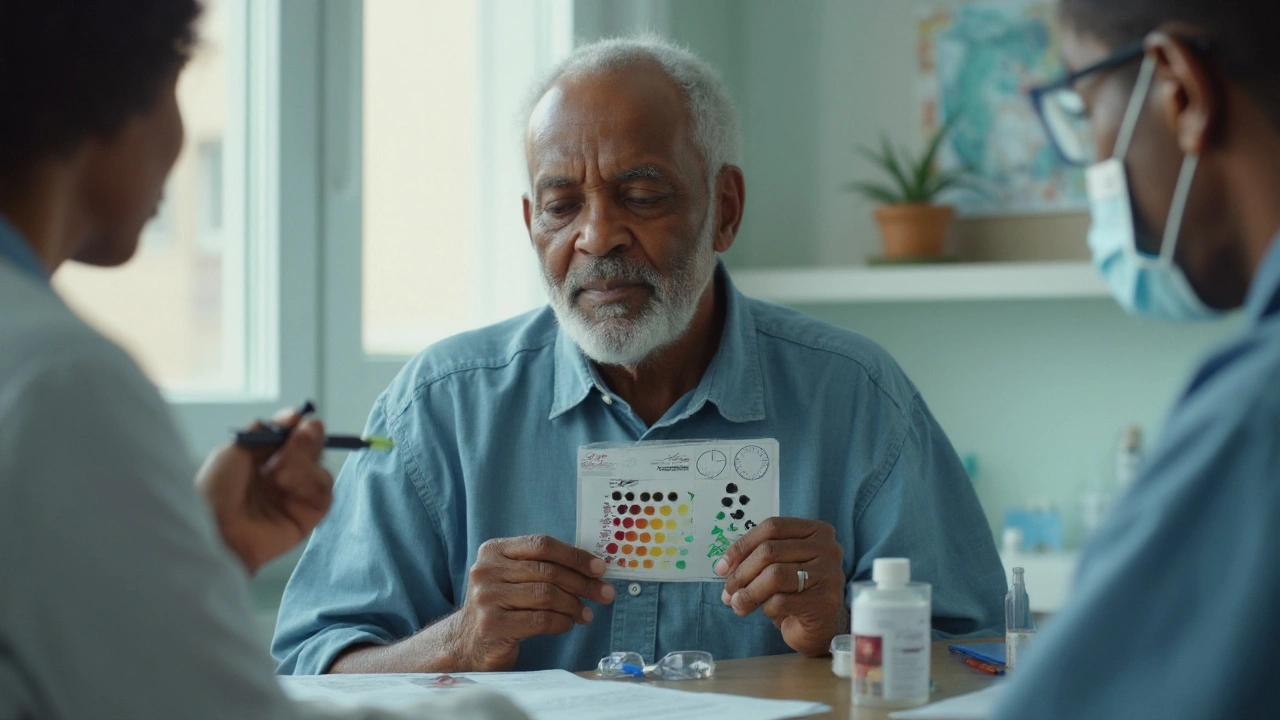
- Always screen vision before and during ethambutol in any context: ask about visual acuity and red-green color changes; dose-adjust in kidney disease.
What 2025 guidelines say (and why ethambutol isn’t there)
Ethambutol has a clear job in active TB: back up rifampin and isoniazid during the intensive phase while you wait on susceptibility tests. It blocks arabinosyl transferase in the mycobacterial cell wall, but it’s bacteriostatic, not strongly sterilizing. That’s one reason it doesn’t earn a seat in LTBI therapy, which aims to sterilize sparse, slow-growing bacilli.
Current guidance across major bodies is consistent:
- CDC/NTCA LTBI guidelines (2020, reaffirmed in updates): preferred regimens are 3HP (once-weekly isoniazid + rifapentine for 3 months), 4R (daily rifampin for 4 months), and 3HR (daily isoniazid + rifampin for 3 months). Alternatives: 6-9 months of isoniazid. Ethambutol is not recommended for LTBI.
- WHO consolidated TB guidelines (2020-2022 updates): options include 3HP, 1HP (1 month of daily isoniazid + rifapentine), 3HR, 6H/9H, and 4R depending on age, HIV status, and drug interactions. Again, ethambutol is absent from the standard LTBI list.
- South Africa (2023-2025 program practice): 3HP is widely used, with 1HP scaling up, especially for people living with HIV on compatible ART. Isoniazid 6H remains for pregnancy and specific cases. No routine ethambutol in LTBI.
Why the consensus? Three reasons that matter in real life:
- Evidence: Trials show strong prevention with rifamycin- and isoniazid-based regimens. There’s no solid evidence that ethambutol adds value for LTBI.
- Safety and practicality: Ethambutol brings optic neuritis risk that needs vision monitoring. That’s hard to scale in routine LTBI care and risk isn’t justified without clear benefit.
- Program fit: LTBI programs are built around short, tolerable regimens that patients finish. Ethambutol doesn’t help that goal.
Authoritative sources behind these statements include CDC/NTCA LTBI Guidelines (2020), WHO consolidated TB guidelines and operational handbooks (2020-2022), ATS/CDC/IDSA treatment of drug-susceptible TB (2016) for the pharmacologic role of ethambutol, and South African National TB Prevention Treatment guidance through 2024.
Edge cases: MDR/XDR exposures and program realities
This is where people get stuck: what if the source case has drug-resistant TB? Can ethambutol play a part in preventive therapy then?
Here’s the grounded answer:
- Contacts of INH-resistant, rifampin-susceptible TB: 4 months of rifampin (4R) is preferred. No ethambutol.
- Contacts of rifampin-resistant, isoniazid-susceptible TB: many programs use 6-9 months of isoniazid (6-9H). No ethambutol.
- Contacts of MDR/RR-TB (resistant to at least isoniazid and rifampin): WHO now supports levofloxacin-based preventive therapy for 6 months when the source strain is susceptible to fluoroquinolones. Randomized trials in adults and children (e.g., V-QUIN, TB-CHAMP, 2020-2023) showed reduced progression to active TB. Ethambutol is not the backbone here.
Could an expert add ethambutol to a fluoroquinolone for MDR-LTBI? Maybe, but it’s uncommon. If used, it’s usually because the source strain is susceptible and the team wants a second companion drug due to high risk, intense exposure, or uncertainty about resistance. Even then, decisions are individualized, time-limited, and monitored closely by a TB specialist. Some programs would pick other companion agents (e.g., ethionamide in certain contexts) instead of ethambutol because of the vision monitoring burden.
Practical context from high-burden settings like South Africa: supply chains, clinic workflows, and vision screening capacity matter. Rolling out a levofloxacin-based regimen with careful safety checks is realistic; adding ethambutol means regular visual checks, which can slow everything down. The juice often isn’t worth the squeeze.
Risk trade-offs to keep in mind if you’re even considering ethambutol in preventive therapy for MDR exposure:
- Toxicity: optic neuritis risk rises with dose and duration; higher at 20-25 mg/kg/day and longer courses.
- Monitoring: baseline and monthly visual checks (acuity and red-green color) are advised; that’s hard with young children.
- Renal function: ethambutol is renally cleared; dose adjust or extend the dosing interval in eGFR <60 mL/min/1.73 m².
- Pregnancy: while ethambutol is used in active TB when needed, preventive therapy doesn’t usually need it; safer to stick to recommended LTBI regimens.
Bottom line in resistant exposures: consult a TB expert. If the strain is fluoroquinolone-susceptible, 6 months of levofloxacin is the center. Ethambutol is usually left on the bench.
How to decide: step-by-step and safety tips
Here’s a simple path I’ve used and taught, built for clinic speed. It works for adults and kids, with the usual adjustments.
Step 1: Confirm LTBI and rule out active TB
- Symptoms: cough, fever, weight loss, night sweats? If yes, evaluate for active TB first.
- Exposure history: Who’s the source case? Any drug resistance known?
- Tests: TB skin test or IGRA positive? Chest radiograph normal? That supports LTBI.
Step 2: Pick the simplest proven regimen the patient can finish
- 3HP (weekly isoniazid + rifapentine for 12 doses) if drug interactions allow and age ≥2 years.
- 4R (daily rifampin for 4 months) if rifapentine isn’t available or interactions block 3HP.
- 3HR (daily isoniazid + rifampin for 3 months) when 3HP isn’t a fit but rifampin is fine.
- 1HP (daily isoniazid + rifapentine for 1 month) where supported by program policy and drug interactions allow-popular for people living with HIV on compatible ART.
- 6-9H (isoniazid alone) if rifamycins are off the table (e.g., certain ART, transplant drugs, severe rifamycin intolerance, pregnancy in programs that avoid rifapentine).
Note: Do not swap in ethambutol if rifamycins or isoniazid don’t fit. It won’t do the job for LTBI.
Step 3: Adjust for drug resistance
- INH-resistant, RIF-susceptible source: choose 4R.
- RIF-resistant, INH-susceptible source: choose 6-9H.
- MDR/RR source: discuss 6 months of levofloxacin with a TB expert. Consider child-friendly formulations for kids. Ethambutol is rarely needed and should not be used alone.
Step 4: Safety screening
- Liver risk: check baseline ALT/AST if HIV-positive, pregnant or postpartum, heavy alcohol use, chronic liver disease, or on hepatotoxic meds.
- Drug interactions: rifamycins hit warfarin, many ARVs, hormonal contraception, azoles, calcineurin inhibitors. Check before starting.
- Renal function: matters if you’re considering ethambutol in any context; dose-adjust or avoid.
- Vision screen: only needed if ethambutol is used for any reason. Ask about visual acuity and color vision; get baseline testing if possible.
Step 5: Make it easy to finish
- Shorter regimens win-3HP, 4R, 1HP-because people complete them.
- Set a finish line date and put it in the patient’s phone.
- Use fixed-dose combinations and once-weekly dosing when available.
- Simple side effect plan: for 3HP/4R, warn about orange urine and potential mild flu-like symptoms; for INH, discuss neuropathy and give pyridoxine (vitamin B6).
Pro tips and pitfalls
- Pro tip: When ART or transplant meds block rifamycins, 6-9H is usually safer than trying to engineer a workaround with second-line drugs.
- Pro tip: If you’re forced to consider MDR-LTBI regimens, get the source isolate susceptibilities. A clear levofloxacin “S” makes life simpler.
- Pitfall: Don’t treat presumed LTBI with ethambutol monotherapy. That’s not preventive therapy.
- Pitfall: Starting ethambutol without a way to monitor vision in kids. If you can’t screen, don’t start it.
Safety quick notes on ethambutol (if used at all)
- Dose (adults in active TB): 15-20 mg/kg daily; toxicity rises above 20 mg/kg/day. For preventive therapy, if used as a companion, experts keep to the lower end and shorter duration.
- Optic neuritis: painless blurring, central scotomas, and red-green color loss. Risk increases with higher dose, longer duration, and renal impairment.
- Renal dosing: extend dosing interval or reduce dose if eGFR <60; avoid in severe renal failure if monitoring is not possible.
- Pregnancy and breastfeeding: acceptable in active TB when needed; for LTBI, pick guideline-backed regimens instead of adding ethambutol.

Quick tables, checklists, FAQs, and next steps
Here’s the part you can screenshot or stick on your clinic wall.
| LTBI Regimen (2025) | Duration | Main Use Cases | Includes Ethambutol? | Key Notes |
|---|---|---|---|---|
| 3HP (INH + rifapentine, weekly) | 3 months (12 doses) | Adults/kids ≥2, if drug interactions allow | No | High completion; watch rifamycin interactions. |
| 4R (rifampin daily) | 4 months | Alternative when 3HP not suitable | No | Few hepatotoxic events; lots of drug interactions. |
| 3HR (INH + rifampin daily) | 3 months | When 3HP/4R not options | No | Short, effective; still has rifampin interactions. |
| 1HP (INH + rifapentine daily) | 1 month | Where supported (often PLHIV on compatible ART) | No | Very short; check local policy and supply. |
| 6-9H (isoniazid daily) | 6-9 months | When rifamycins contraindicated | No | Add vitamin B6; monitor liver risk groups. |
| Levofloxacin (MDR/RR-TB contacts) | 6 months | When source strain is FQ-susceptible | No (rarely added as companion) | WHO-supported for MDR contacts; monitor QT and tendons. |
Checklist: Before starting any LTBI regimen
- Confirm no active TB symptoms; if unsure, get a chest radiograph and sputum tests as indicated.
- Check source case resistance pattern if known; it changes the plan.
- Drug interaction review (rifamycins are the big one).
- Baseline labs if risk for hepatotoxicity; pregnancy test if relevant.
- HIV status known? Adjust regimen if on ART.
- Plan for adherence: dosing calendar, reminders, and a finish date.
Checklist: If ethambutol is ever used (edge cases)
- Confirm the reason: MDR exposure, expert consult, strain susceptible.
- Vision baseline: ask about visual acuity and color vision; formal testing if possible.
- Renal function: get eGFR; adjust dose/interval if reduced.
- Counsel on symptoms: blurred vision, color changes-stop and report immediately.
- Monthly review: vision check, adherence, side effects.
Mini-FAQ
- Can I use ethambutol instead of rifampin or isoniazid for LTBI?
No. It doesn’t prevent TB the way standard LTBI drugs do and adds vision risk. - What if my patient can’t take rifamycins?
Use isoniazid for 6-9 months with vitamin B6. Do not swap in ethambutol. - Any role for ethambutol in MDR-TB contacts?
Rarely, as a companion to a fluoroquinolone under expert guidance. The backbone is levofloxacin if the strain is susceptible. - Is ethambutol safe in pregnancy?
It’s used in active TB when needed, but for LTBI, stick to guideline-backed options (often isoniazid; some programs defer rifapentine in pregnancy). - How do I monitor for ethambutol toxicity?
Ask monthly about vision, check color vision and acuity when possible, and adjust for kidney disease. - What about kids?
Even harder to monitor vision changes. Another reason ethambutol isn’t a good fit for LTBI in children. Choose short rifamycin-based regimens or isoniazid per age and policy.
Next steps and troubleshooting
- If you’re a clinician in a high-burden area: Default to 3HP or 4R when drug interactions allow. For MDR exposures, line up a levofloxacin plan, ECG if needed, and a clear follow-up schedule. Only consider ethambutol if a TB specialist recommends it for a specific reason.
- If you’re managing a TB program: Keep rifapentine and rifampin supply stable; train on interaction checks; add a simple levofloxacin MDR-LTBI protocol. Avoid adding ethambutol to preventive therapy pathways-vision monitoring is heavy and the benefit is weak.
- If you’re a patient or caregiver: Ask which regimen you’re on and how long it lasts. If someone mentions ethambutol for LTBI, ask why, and whether a TB specialist recommended it. Report any vision changes right away.
- Hard scenario: rifamycins off the table, INH intolerance too. This is rare. Don’t improvise with ethambutol monotherapy. Pause, consult an expert, and consider watchful waiting with close follow-up or a tailored regimen based on risk and resistance data.
- Hard scenario: child exposed to MDR-TB and parent worried about quinolones. Share that randomized trials in children support levofloxacin preventive therapy and that it’s now backed by WHO. Discuss risks plainly (tendon, QT) and set monitoring. Ethambutol won’t solve the core need here.
Evidence signposts (no links, names you can look up)
- CDC/NTCA LTBI Treatment Guidelines (2020, updates through 2024)
- WHO Consolidated Guidelines on TB and Operational Handbooks (2020-2022)
- ATS/CDC/IDSA Treatment of Drug-Susceptible TB (2016) for the pharmacology and role of ethambutol in active disease
- Randomized trials on MDR-LTBI prophylaxis: V-QUIN (adults), TB-CHAMP (children), published 2020-2023
- South African National TB Preventive Treatment guidance (2023-2024) on 3HP/1HP scale-up
One last pragmatic note from clinic life in Durban: people finish what feels doable. Short-course rifamycin regimens changed the LTBI game because they’re easy to complete. Ethambutol doesn’t make LTBI simpler, safer, or shorter-so it stays out, except for the rarest expert-led cases.






Oh sweet mercy, another post that treats ethambutol like it’s some kind of TB Swiss Army knife. 🙄 Let’s be real-this isn’t medicine, it’s architectural engineering with bacteria. Ethambutol’s whole raison d’être is being the quiet, slightly creepy backup dancer in active TB’s disco. In LTBI? It’s not even invited to the party. The fact that people still entertain this idea is like asking a potted plant to run a marathon. Optic neuritis? Please. We’ve got 3HP, 4R, 1HP-all elegant, all effective, zero vision nightmares. Ethambutol belongs in a museum next to leeches and bloodletting. 🏛️
From a pharmacokinetic standpoint, ethambutol’s bacteriostatic profile and poor sterilizing activity against dormant bacilli make it pharmacologically inert in LTBI contexts. The mycobacterial dormancy phenotype reduces metabolic activity, rendering cell wall synthesis inhibitors like ethambutol ineffective-unlike rifamycins, which target RNA polymerase and disrupt transcriptional resilience in persister populations. Moreover, the therapeutic index for ethambutol in preventive regimens is unfavorable due to dose-dependent optic neuropathy risk, which scales nonlinearly with renal clearance. The WHO’s shift toward fluoroquinolone-based MDR-LTBI prophylaxis reflects a paradigmatic evolution toward targeted, sterilizing agents with better CNS penetration and lower toxicity burden. This isn’t just guideline adherence-it’s precision medicine.
I CAN’T BELIEVE THIS POST ISN’T MORE OUTRAGED!!! PEOPLE ARE STILL EVEN CONSIDERING ETHAMBUTOL FOR LTBI?!?!?!!! 😱 It’s not just ‘rare’-it’s a medical horror story waiting to happen. Vision loss?! For a *latent* infection?! That’s like using a flamethrower to light a candle. Who’s prescribing this?! Are we running out of doctors?! Or just common sense?! 🚨 I’ve seen patients go blind from this and it’s NOT worth it. STOP. IT. NOW. 🙏 #EthambutolIsNotYourFriend #LTBISafetyFirst
you know what’s wild? 🤔 we’ve got this whole system built around killing TB before it wakes up… but we still treat it like it’s a villain in a movie that needs a whole army. ethambutol? it’s the guy who shows up with a water gun to a dragon fight. 🐉💧 the real magic is in the short regimens-3hp, 1hp-they’re like giving your immune system a nudge, not a sledgehammer. and yeah, vision checks? sure, if you’re doing something risky. but why risk it at all? we’re overcomplicating something that should be simple. 🤷♂️ also, if you’re worried about kids and vision? just don’t use ethambutol. duh. 💙
so let me get this straight-some guy in africa says use levofloxacin and we’re supposed to just throw out ethambutol like it’s trash? 😒 we invented antibiotics, dammit. we don’t follow WHO’s feel-good pamphlets. ethambutol’s been around since the 60s and it WORKS. if you’re too lazy to do vision checks, that’s YOUR problem, not the drug’s. we’ve got real TB problems here-not some ‘program fit’ nonsense. america doesn’t need to copy every UN guideline. we do things better. and if that means using ethambutol in MDR cases? then we should. 🇺🇸 #AmericaFirstTB #EthambutolStillWorks
It’s worth noting that the exclusion of ethambutol from LTBI guidelines isn’t merely a function of evidence-or even toxicity-but a structural optimization of clinical utility within resource-constrained systems. The decision matrix isn’t binary: drug efficacy versus side effects. It’s a trilemma: efficacy, scalability, and compliance. Ethambutol, despite its theoretical utility in MDR-LTBI as a companion agent, introduces a non-linear burden: mandatory serial visual acuity testing, renal dose adjustment protocols, patient education on subtle symptom progression, and the psychological burden of monitoring for irreversible blindness-all for a marginal reduction in progression risk that has not been statistically validated in prospective, population-level trials. Meanwhile, fluoroquinolone regimens, while carrying their own risks (QT prolongation, tendon rupture), are easier to standardize, monitor via routine labs, and integrate into primary care workflows. The absence of ethambutol isn’t negligence; it’s the product of systems thinking in public health. To advocate for its reintroduction is to prioritize pharmacological idealism over epidemiological pragmatism.