Every year, thousands of people overdose on sedatives and sleep medications - not because they’re trying to end their lives, but because they didn’t realize how quickly things could go wrong. A friend falls asleep too hard. A parent takes an extra pill because they’re still awake. Someone mixes a sleeping pill with a drink. What starts as a simple mistake can turn deadly in minutes. The problem? Most people don’t know what to look for.
What Happens When You Overdose on Sedatives?
Sedatives and sleep meds - like Ambien, Xanax, Valium, and even over-the-counter pills like Tylenol PM - slow down your brain and nervous system. That’s why they help you sleep. But when too much gets into your body, they don’t just make you drowsy. They shut down your breathing. And once breathing stops, your brain doesn’t get oxygen. Within minutes, you can slip into a coma. Or worse.The most dangerous part? You won’t always look like you’re in trouble. Someone might just seem "really tired," "out of it," or "sleeping too deep." But if they can’t wake up - no matter how hard you shake them - that’s not sleep. That’s overdose.
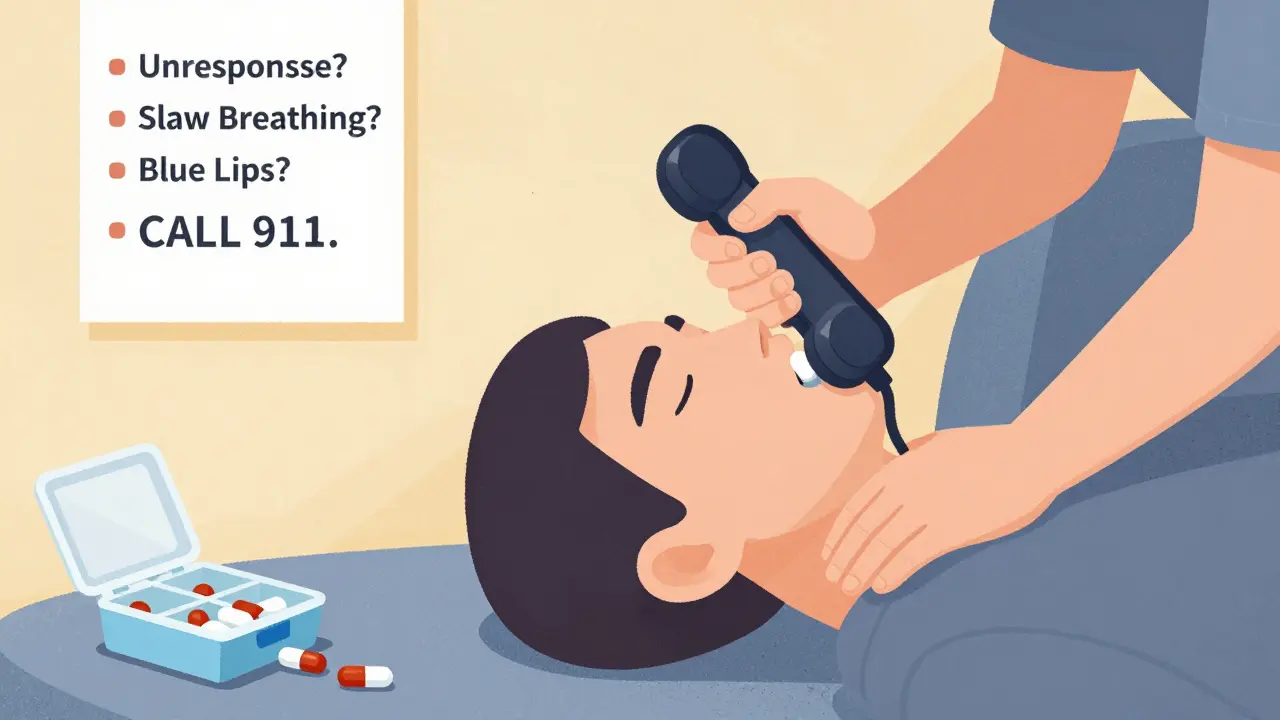
The Warning Signs You Can’t Ignore
There are clear, measurable signs that an overdose is happening. You don’t need medical training to spot them. Here’s what to watch for:- Unresponsiveness: Shout their name. Shake their shoulder. Stomp your foot. If they don’t react at all, even to pain (like a firm pinch on the sternum), they’re not sleeping - they’re in danger.
- Slowed or shallow breathing: Count their breaths for 30 seconds. If they take fewer than 6 breaths in that time (less than 12 per minute), their breathing is dangerously slow. Normal is 12-20. Below 8? This is a medical emergency.
- Cyanosis: Look at their lips, fingertips, and nail beds. If they’re blue or gray, their body isn’t getting enough oxygen. This is a late but unmistakable sign.
- Slurred speech or inability to speak: If they’re awake but can’t form words, or their speech sounds thick and slow, their brain is being suppressed.
- Loss of coordination: They can’t stand, walk, or hold their head up. They stumble like they’re drunk - even if they haven’t had alcohol.
- Cold, clammy skin: Their body temperature drops. Their skin feels wet and cold to the touch. This signals their system is shutting down.
These signs don’t always show up at once. Often, they creep in slowly. That’s why people delay calling 911. They think, "They’ll wake up soon." But every minute counts. Studies show that for every minute you wait after breathing drops below 8 per minute, the chance of survival drops by 7-10%.
Different Medications, Different Risks
Not all sleep meds are the same. Knowing which one was taken helps you understand the danger.- Benzodiazepines (Xanax, Valium, Klonopin): These are the most common culprits. They cause deep sedation but often leave vital signs (heart rate, blood pressure) normal until it’s too late. Overdose deaths from these are up 218% since 2010.
- Z-drugs (Ambien, Lunesta, Sonata): Marketed as safer, but they can still cause fatal respiratory depression. Many people don’t realize these are just as dangerous as benzos when misused.
- Barbiturates (phenobarbital): Rare today, but still prescribed in some cases. These are far more deadly at lower doses. Even a small extra dose can stop breathing.
- Over-the-counter sleep aids (Tylenol PM, Benadryl): These contain diphenhydramine. An overdose doesn’t always cause breathing to stop - but it can cause seizures, hallucinations, rapid heartbeat, and extreme confusion. It’s still life-threatening.
- Melatonin: This is the exception. Even massive doses (like 240mg) rarely cause serious harm. It won’t stop your breathing. But if someone took melatonin along with other meds, don’t assume it’s safe.
The biggest risk? Mixing sedatives with alcohol or opioids. Alcohol alone slows breathing. Opioids do too. Together? They multiply the effect. In 2021, nearly a quarter of benzodiazepine overdose deaths also involved fentanyl. That combination is a death sentence without immediate help.

What to Do Right Now
If you suspect an overdose, don’t wait. Don’t try to "wake them up" with cold water or coffee. Don’t leave them alone. Don’t assume they’ll be fine in the morning.- Check responsiveness: Shout their name. Shake them. Pinch their sternum. If no response, move to step two.
- Check breathing: Look at their chest. Count breaths for 30 seconds. If it’s less than 6, call 911 now.
- Call 911 immediately: Say: "I think someone overdosed on sleep medication." Give your location. Stay on the line.
- Start rescue breathing if needed: If they’re not breathing or taking fewer than one breath every 5 seconds, begin rescue breaths. Tilt their head back, pinch their nose, give one breath every 5 seconds. Don’t stop until help arrives.
- Don’t give them anything to eat, drink, or take: No ipecac. No water. No flumazenil. That’s a drug that reverses benzos - but it can cause seizures if the person is dependent on them. Only trained medics should use it.
- Save the pill bottle: Bring it to the hospital. Tell medics what was taken, how much, and when.
Time is everything. In one study, bystanders waited an average of 47 minutes before calling for help - because they thought the person was just "really tired." That delay cost lives.
What Not to Do
There are dangerous myths about sedative overdoses:- Myth: "They’re just sleeping. Let them rest." Truth: They’re not sleeping. They’re dying.
- Myth: "I’ll just wait and see if they wake up." Truth: By the time they wake up, it’s too late.
- Myth: "Flumazenil will fix this." Truth: It’s dangerous outside a hospital. Never give it yourself.
- Myth: "Only addicts overdose." Truth: Most overdoses happen to people taking their prescribed dose, accidentally doubling up, or mixing with alcohol.
Who’s at Risk?
You might think only people with addiction are in danger. But the data says otherwise.- 9.5 million Americans misused prescription sedatives in 2021.
- 58% of overdoses happen at home - often with family or roommates nearby.
- 72% of cases involve people under 40.
- West Virginia has the highest overdose rate - 3.8 deaths per 100,000 people.
- Even people taking their medication as prescribed can overdose if they drink alcohol, have liver problems, or take other depressants.
It’s not about being "responsible" or "not an addict." It’s about how these drugs work. They’re powerful. And they don’t care if you meant to take one pill or two.
How to Prevent It
Prevention starts with awareness:- Never mix sedatives with alcohol or opioids - ever.
- Store pills in a locked box. Out of reach of teens and others who might take them "just once."
- Use a pill organizer with alarms if you take multiple meds.
- Ask your doctor: "Is this the lowest effective dose?" Many people are on way more than they need.
- Keep naloxone (Narcan) on hand if you or someone you know uses opioids - it won’t reverse sedatives, but it might save a life if opioids are involved.
- Know the signs. Teach your family. Post the checklist on the fridge.
California’s "Don’t Die" campaign gave out 250,000 overdose recognition cards to pharmacies. People who used them were 22% more likely to call 911 in time. Knowledge saves lives.
Final Thought
You don’t need to be a doctor to recognize a sedative overdose. You just need to know what to look for - and act fast. If someone can’t wake up, isn’t breathing right, or looks blue - don’t wait. Don’t hesitate. Call 911. Give rescue breaths. Stay with them.It’s not dramatic. It’s not heroic. It’s simple. And it might be the only thing that keeps someone alive.
Can you overdose on over-the-counter sleep aids like Tylenol PM?
Yes. Tylenol PM and similar products contain diphenhydramine, an antihistamine that can cause dangerous side effects at high doses - including seizures, hallucinations, rapid heartbeat, and extreme confusion. While it doesn’t usually stop breathing like prescription sedatives, it can still lead to coma and death, especially in children or when mixed with alcohol.
Does flumazenil reverse sedative overdoses?
Flumazenil can reverse benzodiazepine overdoses, but it’s only safe to use in a hospital. If someone has been taking these drugs regularly, flumazenil can trigger sudden seizures or heart problems. Never give it yourself. Emergency responders are trained to use it safely.
Is melatonin dangerous in large doses?
Melatonin is one of the safest sleep aids. Even doses 60 times higher than normal (like 240mg) rarely cause serious harm. The worst effects are headaches, dizziness, or nausea - not respiratory failure. But if someone took melatonin with other drugs, assume the worst and seek help.
What’s the difference between sedative overdose and opioid overdose?
Opioid overdoses usually cause pinpoint pupils, extreme drowsiness, and slow breathing. Sedative overdoses often have normal-sized pupils and may not show obvious signs until breathing drops. But if both are mixed - which is common - the signs blur. Always assume the worst and call 911.
Can you survive a sedative overdose without medical help?
Survival without help is extremely rare. Once breathing drops below 8 breaths per minute, brain damage starts within minutes. Most people who survive had immediate medical intervention - including oxygen, breathing support, and IV fluids. Delaying care increases the risk of permanent damage or death.
Why do people wait so long to call 911 during a sedative overdose?
Because the symptoms look like deep sleep. People think, "They’re just exhausted," or "They had a long day." Bystanders often misread slurred speech as drunkenness or confusion as normal tiredness. A 2022 study found that 68% of bystanders delayed calling for help because they didn’t recognize the signs as an emergency.
Are newer sleep meds like Ambien safer than older ones?
No. Z-drugs like Ambien were marketed as safer alternatives to benzodiazepines, but studies show they carry the same risk of respiratory depression - especially when mixed with alcohol or taken in higher doses. The FDA added boxed warnings to these drugs in 2023 after hundreds of overdose deaths.
What should I do if I find an empty pill bottle next to someone who’s unconscious?
Call 911 immediately. Don’t wait. Don’t try to figure out what was taken. Take the bottle with you to the hospital. Even if you’re not sure, the medics need that information to treat the person correctly. Time is the most critical factor.





Dude just passed out from Ambien. I thought he was snoring. Turned out he was blue. Called 911. He’s fine now. Don’t wait.
I used to think sleep meds were harmless... until my cousin took two Tylenol PMs because she was "stressed" and ended up in the ER with hallucinations. These aren’t candy. They’re silent killers wrapped in beige capsules. We need better labeling. Like, actual warning labels that scream, not whisper.
You know what’s terrifying? The fact that we’ve normalized this. We’ve turned sedatives into bedtime tea. We take them like they’re vitamins. We mix them with wine like it’s a cocktail recipe. And then we act shocked when someone doesn’t wake up. But here’s the truth - it’s not about willpower, it’s about neurochemistry. These drugs don’t negotiate. They don’t care if you’re a good person. They don’t care if you meant to take one. They just shut down the lights. And the worst part? You won’t even know you’re dying until it’s too late. Your brain doesn’t panic. It just... stops. And you’re left there, breathing at 5 per minute, while your roommate scrolls TikTok thinking you’re just tired.
Y’all need to stop sleeping on this. I taught my whole family the breathing count trick. Now my mom keeps a checklist taped to her medicine cabinet. If you’re not checking breaths, you’re not helping. Be the person who saves the day. Not the one who says "they’ll wake up."
flumazenil? lol. like i’m gonna keep that in my junk drawer next to the expired ibuprofen. jk. but seriously, if you think you can just pop a pill to fix this, you’re the reason people die.
I’ve been a nurse for 17 years... and I still get chills reading this. I’ve seen the same thing over and over: someone’s mom, brother, roommate - just... gone - because no one knew what to look for. The silence after the last breath... it haunts you. Please. Share this. Print it. Put it on the fridge. Save a life.
I used to roll my eyes at people who said "sleep meds are dangerous." Then my sister took a Z-drug with a glass of wine and ended up in ICU for 3 days. She doesn’t even remember it. That’s the problem. You don’t feel it coming. You just... disappear. I keep Narcan at home now. Not for opioids - for the times someone might’ve mixed it with something else. Better safe than sorry.
In India, many elderly take sleep pills because they’re cheap and easy to get. No one tells them the risks. I showed my aunt this list. She cried and said, "I didn’t know I was killing myself slowly." I printed copies for her friends. Small acts matter.
Ah yes... the classic "knowledge saves lives" narrative. How quaint. As if awareness alone can counteract the neoliberal commodification of mental health, the pharmaceutical industry’s engineered dependency, and the systemic erasure of holistic sleep hygiene in favor of chemical band-aids. We’re not just talking about pills - we’re talking about the collapse of the human capacity to rest without pharmacological mediation. And yet... you still think a checklist on the fridge will fix it?
i didnt even know tylenol pm could do that. my mom takes 2 every night. im gonna talk to her. also... typo on the post? "breathing drops below 8" - did you mean 8 per minute? just wanna be sure lol
I used to think if you didn’t take a bunch, you were fine. Then my friend’s dad took one extra pill because he was still awake. He never woke up. No drama. No struggle. Just... gone. Don’t wait for a sign. If they’re not responding, call 911. No excuses.
Oh wow. Another PSA. So, what? People are dumb? Maybe if they didn’t take drugs they wouldn’t overdose? Maybe the real problem is people who can’t handle their own lives? Just saying.
i think melatonin is the real villain here 😅. everyone thinks it's "natural" so they take 10mg and then blame the Ambien when they hallucinate. also... why is everyone so scared of breathing? we all breathe... right? 🤔
my roommate took a xanax and passed out. i thought he was just sleeping it off. i didnt know what to do. i just sat there. i still feel bad. this post... it’s the thing i needed to see. thanks.
This is the most important public health message I’ve read in years. I’ve shared it with my yoga studio, my book club, even my neighbor’s teenage son who’s been experimenting with his dad’s sleep meds. Knowledge isn’t power - it’s a lifeline. Thank you for writing this with clarity, not fear. We need more of this.