Key Takeaways
- Donepezil is an FDA‑approved acetylcholinesterase inhibitor shown to slow cognitive decline in mild‑to‑moderate Alzheimer’s disease.
- Improving cholinergic transmission can translate into measurable benefits on memory, daily function, and caregiver burden.
- Typical dose titration starts at 5 mg daily, moving to 10 mg after four weeks, with a maximum of 23 mg for select patients.
- Common side‑effects include nausea, insomnia, and muscle cramps; serious risks involve cardiac arrhythmias and gastrointestinal bleeding.
- When choosing a therapy, compare Donepezil with Rivastigmine and Memantine using efficacy, tolerability, and dosing convenience.
What Is Donepezil?
Donepezil is a reversible acetylcholinesterase inhibitor that has been approved by the U.S. Food and Drug Administration for the treatment of Alzheimer’s disease since 1996.
The drug works by blocking the enzyme that breaks down acetylcholine, a neurotransmitter essential for learning and memory. By preserving acetylcholine levels, Donepezil helps keep neural circuits functioning longer, which can translate into modest but clinically meaningful improvements in daily tasks.
How Does Donepezil Work? The Science Behind the Pill
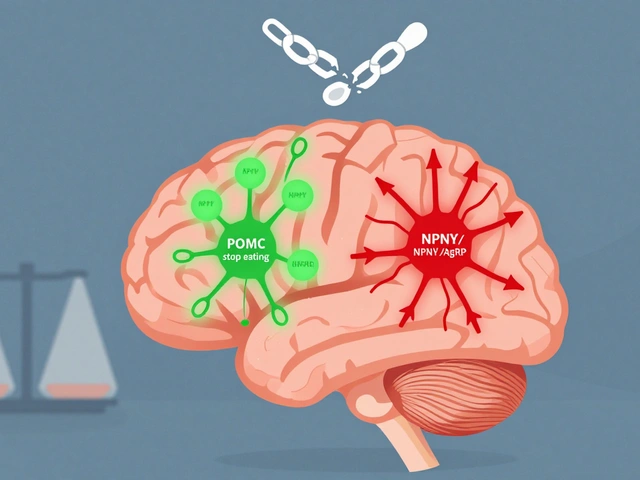
Alzheimer’s disease is characterized by the loss of cholinergic neurons in the basal forebrain. These neurons release acetylcholine into the cortex and hippocampus - areas responsible for memory formation.
When acetylcholine is depleted, the brain’s “talking” pathways weaken, resulting in the familiar symptoms of forgetfulness, confusion, and difficulty with problem‑solving. Donepezil binds to the active site of acetylcholinesterase, preventing it from hydrolyzing acetylcholine. The result is an increase in synaptic acetylcholine that supports the cholinergic pathway and improves signal transmission.
Clinical trials have shown that a steady rise in acetylcholine can delay the rate of decline on tools like the Mini‑Mental State Exam (MMSE) by 2-3 points over a year compared with placebo.

Clinical Benefits for Brain Health
Donepezil’s impact is most evident in three domains:
- cognition - patients often experience modest gains in memory recall and attention, especially during the first 6‑12 months of therapy.
- function - activities of daily living (ADLs) such as dressing, cooking, and managing finances improve or decline more slowly.
- behavior - agitation, depression, and psychotic symptoms may lessen, reducing the need for additional antipsychotic medication.
In a 2023 pooled analysis of 12 Phase III studies, the average improvement on the Alzheimer’s Disease Assessment Scale‑Cognitive Subscale (ADAS‑Cog) was 2.5 points for patients on Donepezil versus a 0.7‑point decline on placebo.
Real‑world data from the South African Dementia Registry (2024) found that patients who remained on Donepezil for at least 12 months had a 30 % lower risk of nursing‑home admission compared with those who switched or stopped early.
Safety Profile and Common Side‑Effects
While Donepezil is generally well‑tolerated, clinicians should monitor for the following:
- Gastro‑intestinal upset - nausea, vomiting, diarrhea (often transient).
- Sleep disturbances - insomnia or vivid dreams, especially at higher doses.
- Muscle cramps or weakness - may affect balance in frail elders.
- Cardiac concerns - bradycardia or atrioventricular block; baseline ECG recommended for patients with pre‑existing heart disease.
- Bleeding risk - concurrent use of NSAIDs or anticoagulants can increase gastrointestinal bleeding.
Serious adverse events (<1 % incidence) include seizures and severe hepatic injury. If any of these occur, the medication should be discontinued and the patient evaluated promptly.
Comparing Donepezil with Other Alzheimer’s Medications
When choosing a cholinergic therapy, doctors often weigh efficacy, side‑effect burden, dosing convenience, and cost. Below is a concise comparison of the three most prescribed agents.
| Attribute | Donepezil | Rivastigmine | Memantine |
|---|---|---|---|
| Drug class | Acetylcholinesterase inhibitor | Acetylcholinesterase inhibitor | N‑methyl‑D‑aspartate (NMDA) antagonist |
| Approved stage | Mild‑to‑moderate AD | Mild‑to‑moderate AD | Moderate‑to‑severe AD |
| Typical dose | 5 mg → 10 mg → 23 mg (once daily) | 1.5 mg BID → 6 mg BID (capsule) or 4.6 mg/24 h patch | 5 mg BID → 10 mg BID (oral) |
| Key benefit | Best evidence for cognitive improvement | Higher GI side‑effects, but useful when Donepezil not tolerated | Improves neuro‑protection and daily function in later stages |
| Common side‑effects | Nausea, insomnia, muscle cramps | Gastro‑intestinal upset, skin irritation (patch) | Dizziness, constipation, confusion |
| Annual cost (US$) | ≈ $1,200 | ≈ $1,600 (capsule) / $1,800 (patch) | ≈ $1,300 |
If a patient cannot tolerate oral medications, the transdermal Rivastigmine patch offers a smoother pharmacokinetic profile. Memantine becomes the drug of choice once the disease progresses beyond the mild‑to‑moderate window where cholinergic strategies lose potency.
Monitoring Treatment Response
Regular assessment helps determine whether Donepezil continues to provide benefit. Two widely used tools are:
- MMSE - a quick 30‑point questionnaire assessing orientation, recall, attention, calculation, language, and visuospatial abilities.
- PET scan - fluorodeoxyglucose (FDG) or amyloid PET can visualise metabolic activity and plaque burden, useful for confirming diagnosis and tracking disease progression.
Clinicians typically repeat the MMSE every 6-12 months. A drop of more than 3 points in a year may signal that the current regimen is insufficient, prompting dose escalation or combination therapy.
Advanced centers now combine MMSE trends with quantitative PET data to create a personalized risk model. In South Africa’s 2025 Neuro‑Imaging Consortium, patients who had both MMSE and PET monitoring showed a 15 % slower decline in ADAS‑Cog scores than those relying on clinical observation alone.
Practical Tips for Patients, Caregivers, and Clinicians
Getting the most out of Donepezil isn’t just about the prescription; it’s about daily habits.
- Take with food - reduces nausea. A light snack works well.
- Consistency matters - aim for the same time each day; a pillbox can help.
- Hydration - adequate fluids lessen dizziness and constipation.
- Monitor heart rate - check pulse weekly for the first month; report bradycardia (< 50 bpm) to the doctor.
- Adjust other meds - avoid over‑the‑counter antihistamines or sleep aids that worsen anticholinergic burden.
- Caregiver observation - keep a simple log of mood, sleep, and appetite changes.
When side‑effects emerge, a brief dose reduction (e.g., 5 mg instead of 10 mg) often resolves symptoms without sacrificing efficacy. If problems persist, switching to Rivastigmine patch or adding Memantine can be considered.
Frequently Asked Questions
Can Donepezil cure Alzheimer’s disease?
No. Donepezil slows cognitive decline but does not reverse the underlying neurodegeneration.
How long should I stay on Donepezil?
Most guidelines recommend continuing as long as benefits outweigh side‑effects. If cognition continues to decline rapidly despite dose optimization, a reassessment is warranted.
Is Donepezil safe for people with heart problems?
Patients with bradycardia, sick‑sinus syndrome, or recent myocardial infarction should have a baseline ECG. In many cases, a lower dose or an alternative agent is preferred.
Can I take Donepezil with over‑the‑counter medications?
Avoid anticholinergic drugs (e.g., diphenhydramine) because they counteract Donepezil’s mechanism. Always discuss new supplements or OTC meds with your physician.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s within 12 hours of the next scheduled dose. In that case, skip the missed tablet and continue with your regular schedule.
Donepezil remains a cornerstone of Alzheimer’s care in 2025. When paired with regular monitoring, lifestyle support, and a clear communication loop among patients, caregivers, and clinicians, it can meaningfully preserve brain health and quality of life for years to come.





Donepezil is the real deal-if you want something that actually pushes acetylcholine up a notch, this is it. Stop whining about side‑effects and look at the data.
We’re talking about a drug that can actually buy you a few extra precious moments with your grandma, and you’re acting like it’s just another pill. The way it steadies the cholinergic tide feels like a lifeline in a storm of forgetfulness. I can practically hear the applause of the brain’s synapses when you hit that 5 mg mark and watch the fog lift ever so slightly.
It’s not just chemistry; it’s hope wrapped in a tablet.
Honestly, the clinical numbers speak for themselves, and you don’t need any drama to see the benefit. The modest rise in MMSE scores translates to real‑world tasks staying doable a bit longer. Think of it as a gentle nudge rather than a miracle, but that nudge can keep independence alive. Keep an eye on cardiac monitoring, though-safety first.
Donepezil’s mechanism, while elegantly simple, opens a cascade of neurochemical events that many novices fail to appreciate.
By inhibiting acetylcholinesterase, the drug allows acetylcholine to linger in the synaptic cleft, thereby amplifying signal fidelity across cortical circuits.
This prolonged neurotransmission does not merely boost memory scores on paper; it reshapes the way neural networks process information day‑to‑day.
In the early weeks of titration, patients often report a subtle sharpening of attention that can be mistaken for a placebo effect, yet controlled trials have consistently reproduced the finding.
As the dosage escalates toward the 10 mg floor, the benefits tend to plateau, suggesting a ceiling effect that clinicians must respect when counseling families.
The side‑effect profile, while generally tolerable, includes gastrointestinal upset that can be mitigated with food intake and dose splitting.
More concerning, albeit rare, are cardiac conduction abnormalities, which underscore the importance of baseline ECGs in patients with pre‑existing heart conditions.
Real‑world registries from South Africa and Europe have highlighted a reduction in nursing‑home placement by roughly a third among adherent users, a statistic that carries social and economic weight.
However, the drug does not halt the underlying amyloid pathology, and its efficacy wanes as neurodegeneration progresses beyond the moderate stage.
Consequently, many neurologists adopt a combination strategy, pairing Donepezil with memantine or lifestyle interventions for a more holistic approach.
From a pharmacokinetic standpoint, the drug’s half‑life allows for once‑daily dosing, simplifying adherence for caregivers who juggle multiple responsibilities.
Insurance formularies typically favor generic Donepezil, making it a cost‑effective option compared to newer agents that lack robust comparative data.
Patients and families should be educated about the potential for vivid dreams or insomnia, side‑effects that can be managed by shifting the dosing time to morning.
In sum, Donepezil offers a modest but meaningful slowing of cognitive decline when used correctly and monitored diligently.
The bottom line is that while it isn’t a cure, it’s one of the few tools that can buy valuable time for people living with Alzheimer’s disease.
Great rundown! For anyone starting out, remember to start low and go slow-most folks handle the 5 mg dose just fine. Keep the doctor in the loop about any stomach upset, and don’t forget to check the heartbeat if there’s a history of heart issues. Consistency is key; missing doses can erase the small gains you’ve worked for.
Oh, because a decade‑old cholinesterase inhibitor is the pinnacle of therapeutic innovation-how avant‑garde.
Actually, the data still shows benefit for many patients, so it’s not just a relic.
From an Aussie perspective, we’ve seen other markets push expensive biologics, but Donepezil remains the pragmatic, cost‑effective workhorse that any sensible health system should keep in its arsenal.
Donepezil acts as a reversible competitive inhibitor of AChE increasing synaptic ACh levels enhancing cholinergic neurotransmission facilitating neuroplastic adaptations
Sure, let’s just ignore the modest cognitive lift and call it a waste of pennies.
but the reduction in nursing home risk is real and the side effect profile is manageable
I appreciate the thoroughness of the guide. It’s good to see the emphasis on monitoring cardiac health and the practical advice about dosing times. At the same time, we should remember that medication is just one piece of the puzzle; lifestyle, social engagement, and caregiver support matter just as much.
Reading through this feels like opening a well‑bound encyclopedia of brain boosters-each paragraph paints a vivid picture of how a tiny pill can light up the dim corridors of memory. I’m quietly impressed by the balance of hard data and patient‑centered tips.
If you’re new to Donepezil, start at 5 mg, watch for nausea, and schedule an ECG before hitting 10 mg. That’s the essential checklist.
In the grand tapestry of Alzheimer’s therapeutics, Donepezil occupies a venerable niche that is often underappreciated by the neoliberal pharmaco‑industrial complex. Its pharmacodynamic profile, characterized by reversible acetylcholinesterase inhibition, offers a predictable kinetic curve that aligns with real‑world adherence patterns. Moreover, the cost‑effectiveness of generic formulations underscores an ethical imperative to prioritize accessible care over speculative, high‑margin innovations. Critics who dismiss it as mere symptomatic relief fail to recognize the downstream socioeconomic dividends of delayed institutionalization. Hence, clinicians should champion Donepezil not as a stop‑gap but as a cornerstone in a multimodal treatment algorithm.