When your blood sugar climbs too high, your body doesn’t just feel tired-it starts to break down. Hyperglycemia isn’t just a number on a glucose meter. It’s a warning sign that your body can’t use the sugar in your blood, and if left unchecked, it can lead to life-threatening emergencies like diabetic ketoacidosis or hyperosmolar hyperglycemic state. This isn’t something that happens overnight. For many people, it creeps up slowly-fatigue, thirst, frequent urination-until suddenly, they’re confused, vomiting, or struggling to stay awake. And by then, it’s already an emergency.
What Exactly Is Hyperglycemia?
Hyperglycemia means your blood glucose level is higher than normal-typically above 180 mg/dL. It’s not rare. In fact, over 37 million Americans with diabetes deal with it regularly. But it’s not just a diabetes problem. Stress, illness, certain medications like steroids, or even undiagnosed conditions like Cushing’s syndrome can trigger it too.
The root cause is simple: not enough insulin, or insulin that doesn’t work right. In type 1 diabetes, your body doesn’t make insulin at all. In type 2, your cells ignore it. Either way, sugar piles up in your bloodstream instead of fueling your muscles and organs. That’s when symptoms start.
Early Signs You Can’t Ignore
The first red flags are easy to miss because they feel like everyday stuff. You’re thirsty-not just a little, but constantly. You’re drinking more than four liters of water a day and still not satisfied. You’re peeing every hour, even at night. That’s polyuria and polydipsia-medical terms, but the experience is simple: your body’s trying to flush out the extra sugar.
Blurred vision? That’s common. High sugar pulls fluid from your lenses, making it hard to focus. Fatigue? It’s not just a long day. Your cells are starving because they can’t access the glucose floating past them. You might think you’re just burned out from work-but if this lasts more than a couple of days, check your blood sugar.
According to the American Diabetes Association, 68% of people with high blood sugar report blurred vision, and 79% feel extreme tiredness. These aren’t random symptoms. They’re your body screaming for help.
When It Gets Worse: The Intermediate Stage
If your blood sugar climbs past 250 mg/dL, things shift. Headaches become frequent. You can’t concentrate. Simple tasks feel impossible. You might lose weight without trying-even if you’re eating normally. That’s because your body starts breaking down fat and muscle for energy.
One study found 47% of people with type 2 diabetes had trouble focusing when their glucose was above 250 mg/dL. That’s not just brain fog. It’s your brain struggling to function without proper fuel. And if you’re on insulin, you might be tempted to take more. But here’s the trap: taking too much too fast can crash your sugar into hypoglycemia. That’s just as dangerous.
Dr. Robert Vigersky from Mayo Clinic points out that many people miss the dawn phenomenon-a natural sugar spike between 4 and 8 a.m. caused by hormones. If your morning numbers are consistently high, it’s not laziness. It’s your body’s biology. Adjusting your nighttime insulin or basal rate can fix this.
Emergency Mode: When Your Body Starts Shutting Down
When blood sugar hits 300 mg/dL or higher, you’re in danger. Two life-threatening conditions can develop: diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS).
DKA mostly hits people with type 1 diabetes. Your body starts burning fat for fuel, creating toxic acids called ketones. Signs: fruity-smelling breath (like nail polish remover), rapid breathing (more than 24 breaths per minute), nausea, vomiting, and stomach pain. Blood pH drops below 7.3. This can turn deadly in under 24 hours.
HHS is more common in type 2 diabetes, especially in older adults. There are no ketones, but your blood sugar soars past 600 mg/dL. Your blood gets thick and syrupy. You become severely dehydrated-losing 8 to 12 liters of fluid. You might be confused, have weakness on one side of your body, or slip into a coma. Mortality rates for HHS are 15-20%. That’s higher than DKA’s 1-5%.
And here’s the scary part: 67% of patients on DiabetesDaily.com didn’t realize they were in danger until their sugar hit 300 mg/dL or higher. By then, it’s often too late to fix it at home.
What to Do When Blood Sugar Spikes
If your reading is above 240 mg/dL, don’t wait. Act now.
- Check for ketones. Use a urine test strip or a blood ketone meter. If ketones are moderate or high, don’t exercise. You could make things worse.
- Take your fast-acting insulin. Follow your correction factor-usually 1 unit for every 10 to 15 grams of carbs your sugar is above target. Don’t guess. Use your personal ratio.
- Drink water. Eight to 16 ounces every hour. Sugar-free fluids only. No soda, juice, or sports drinks. You’re trying to flush out sugar, not add more.
- Test again in two hours. If your sugar didn’t drop by at least 30-50 mg/dL, call your doctor or go to the ER.
Insulin stacking-taking more insulin too soon-is a common mistake. It causes dangerous lows. Wait at least 4 hours between correction doses unless your doctor says otherwise.
Triggers You Can Control
Most spikes don’t come out of nowhere. They have causes:
- Illness (42% of cases)-colds, flu, infections raise stress hormones that push sugar up.
- Carb mistakes (29%)-eating more than you thought, not counting properly.
- Insulin pump failure (18%)-clogged tubing, disconnected sites, expired insulin.
- Stress (11%)-emotional or physical tension triggers cortisol, which raises blood sugar.
One Reddit user shared how he ignored a spike for two days because he thought he was just “stressed from work.” His sugar hit 520 mg/dL. He ended up in the ER. He’s now on a continuous glucose monitor (CGM) and says it saved his life.
Technology That’s Changing the Game
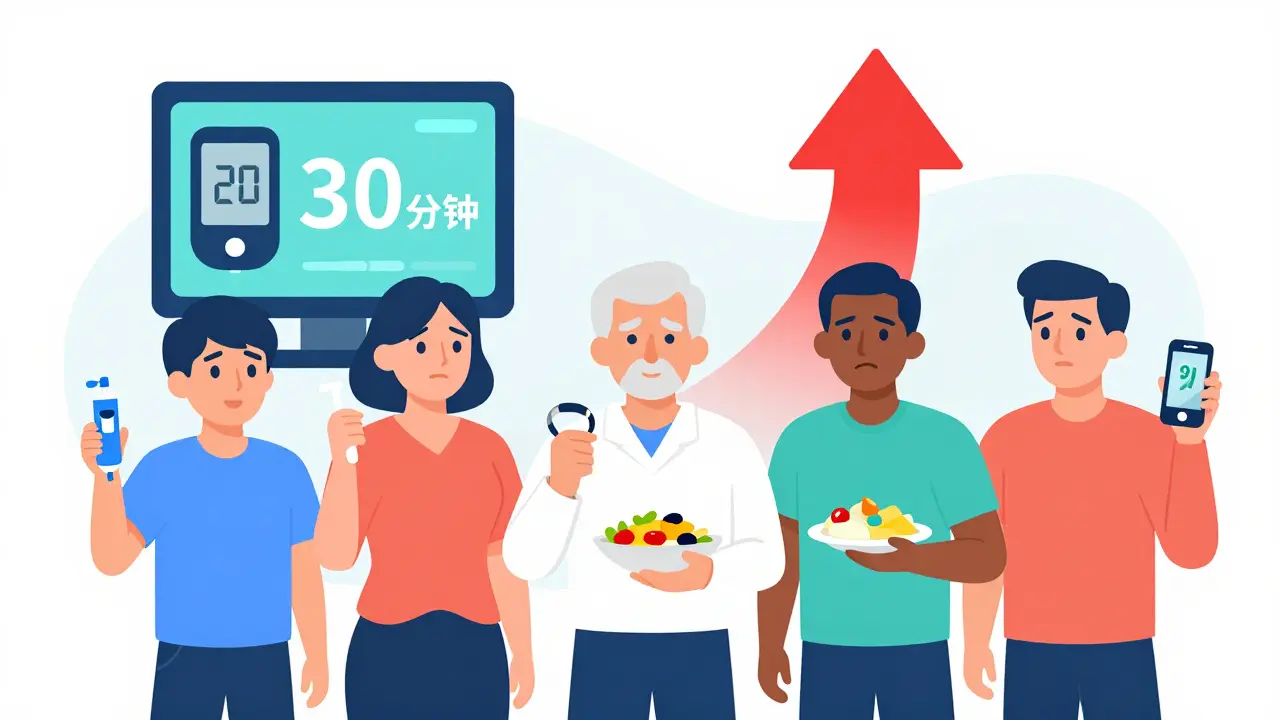
CGMs aren’t just trendy gadgets. They’re lifesavers. A 2023 Dexcom study showed users reduced their hyperglycemia episodes by 57% because they got alerts before numbers got dangerous. The FDA just approved Dexcom G7’s new “Glucose Guardian” feature-it predicts spikes 30 minutes ahead. That’s huge.
People using CGMs respond 74 minutes faster than those relying on fingersticks. That’s the difference between fixing a spike at 280 mg/dL versus letting it hit 450 mg/dL.
And it’s not just about tech. Structured education programs like the CDC’s Diabetes Self-Management Education cut emergency visits by 42%. Learning how to read your numbers, adjust insulin, and recognize early signs makes all the difference.
Who’s at Highest Risk?
Not everyone faces the same danger.
- Children with type 1 diabetes are more likely to develop DKA. It’s the leading cause of death in this group.
- Older adults with type 2 diabetes are far more likely to develop HHS-and have a 22% death rate if they’re over 65.
- Black and low-income patients experience 2.3 times more hyperglycemia emergencies than white patients. Why? Limited access to insulin, CGMs, and education.
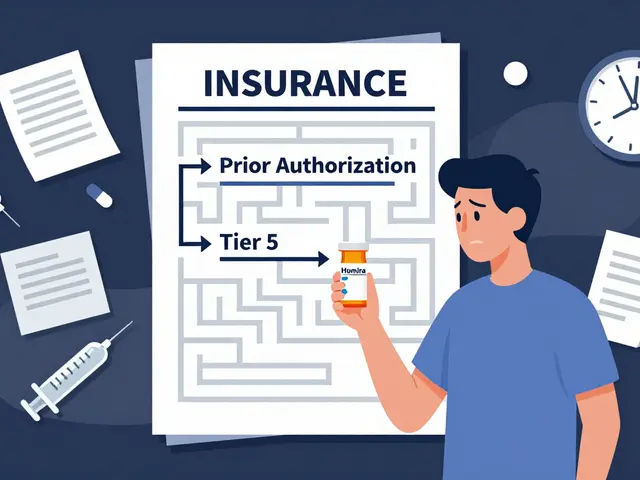
Cost is a silent killer. CGMs cost $1,200 a year. Even with Medicare coverage, copays and supplies add up. Many people skip testing because they can’t afford it. That’s not a personal failure-it’s a system failure.
What to Avoid
Don’t:
- Ignore thirst or frequent urination
- Exercise when ketones are present
- Take extra insulin without checking your correction ratio
- Assume you’re “just tired” or “dehydrated” without testing
- Wait until you’re vomiting or confused to act
Do:
- Keep a log of your high readings and what might’ve caused them
- Have a written emergency plan with your doctor
- Wear a medical ID bracelet
- Teach someone close to you how to give you glucagon or call 911
When to Call 911
Go to the ER immediately if you have:
- Blood sugar over 600 mg/dL
- Confusion, drowsiness, or trouble waking up
- Difficulty breathing or rapid, deep breaths
- Fruity-smelling breath
- Vomiting or abdominal pain
- Weakness on one side of your body
Don’t drive yourself. Call for help. HHS and DKA can kill you faster than you think.
The good news? Most hyperglycemic emergencies are preventable. You don’t need to be perfect. You just need to be aware. Test often. Know your triggers. Act early. And never, ever ignore the signs.
What’s the difference between DKA and HHS?
DKA (diabetic ketoacidosis) happens mostly in type 1 diabetes and involves high blood sugar plus ketones and acid in the blood. Symptoms include fruity breath, vomiting, and rapid breathing. HHS (hyperosmolar hyperglycemic state) occurs in type 2 diabetes, with extremely high blood sugar (often over 600 mg/dL), no ketones, and severe dehydration. HHS causes confusion and coma more often and has a higher death rate.
Can non-diabetics get hyperglycemia?
Yes. Severe stress from trauma, infection, or stroke can cause temporary high blood sugar. Certain medications like steroids, Cushing’s syndrome, or pancreatitis can also trigger it. In these cases, blood sugar usually returns to normal once the underlying issue is treated-but it’s still dangerous and needs medical attention.
Why does my blood sugar spike in the morning?
This is called the dawn phenomenon. Between 4 and 8 a.m., your body releases hormones like cortisol and growth hormone that naturally raise blood sugar. If your insulin doesn’t match this rise, your numbers climb. Adjusting your nighttime basal insulin or using a CGM with predictive alerts can help manage it.
Is it safe to exercise when my blood sugar is high?
Only if your ketones are negative and your sugar is below 300 mg/dL. If ketones are present, exercise can make your blood sugar go even higher and increase the risk of DKA. Test for ketones first. If they’re moderate or high, skip exercise and focus on hydration and insulin.
How can I prevent frequent high blood sugar episodes?
Track your patterns. Keep a log of when highs happen and what you ate, did, or felt before. Use a CGM for real-time alerts. Stick to consistent meal times and insulin schedules. Talk to your doctor about adjusting your basal insulin or correcting for the dawn phenomenon. Education programs like CDC’s Diabetes Self-Management Education can reduce episodes by 42%.
What should I do if I can’t afford insulin or CGMs?
Contact the American Diabetes Association’s 24/7 hotline-they help people find low-cost insulin programs and patient assistance. Some manufacturers offer $35 insulin coupons. Community health centers may provide free or sliding-scale glucose supplies. Never skip insulin because of cost. A single high-blood-sugar emergency can cost over $14,000. Prevention is always cheaper than the hospital.






I ignored my sugar for 3 days once thought i was just tired turned out i was at 520 had to be rushed to er now i wear a cgms its the only thing keeping me alive
I didn't know non-diabetics could get this. My uncle had high sugar after his heart attack. Scary stuff.
In india we dont even have access to test strips half the time how are people supposed to survive this
The data presented here is statistically significant and clinically validated. However, the absence of peer-reviewed citations undermines its credibility.
So let me get this straight... my body is slowly turning into syrup and I'm supposed to just 'drink water' and 'test again'? Like this is a bad yoga class and not a medical emergency?
It's interesting how hyperglycemia exposes the fragility of metabolic homeostasis. The body's inability to process glucose isn't just a biochemical failure-it's a systemic collapse of signaling, feedback, and energy allocation. We treat it like a number, but it's really a cry from the cellular level.
I used to think high blood sugar was just about eating too much cake. Then I watched my mom slip into HHS. She didn't vomit. Didn't have fruity breath. Just got super quiet. Couldn't stand up. That's when I knew-this isn't about discipline. It's about survival. And access. And money. And how broken this system is.
I've been using a CGM for 6 months. The alerts saved me twice. Still can't afford the strips sometimes. But I do what I can.
CGMs are just a scam by Big Pharma to keep you buying gadgets. The real cause? Vaccines and GMO sugar. My cousin’s sugar dropped when he stopped eating 'lab-made carbs'. Just sayin'
I find it deeply troubling that so many people treat this condition with such casual disregard. The fact that individuals are relying on Reddit advice instead of consulting a licensed endocrinologist is not only irresponsible-it's morally indefensible. Your life is not a social media experiment. If you cannot afford insulin, you should have planned better. This isn't a tragedy of circumstance; it's a failure of personal accountability. And yet, we reward ignorance with pity and memes. The system is broken because people refuse to take ownership.
I work in a hospital ER. Seen too many of these cases. People show up with sugar over 800. Some are homeless. Some have insurance but their copay for insulin is $400 a month. They don't choose this. The system chooses for them. And then we act shocked when they end up in ICU. It's not about willpower. It's about who gets to live and who gets to die quietly because they can't afford the cure.