Myasthenia gravis (MG) isn’t just muscle weakness. It’s your body turning against itself-attacking the very connection between nerves and muscles. Imagine trying to lift your eyelid, chew food, or even breathe, but your muscles keep giving out. By midday, your arms feel like lead. By evening, you can’t speak clearly. This isn’t fatigue. It’s myasthenia gravis, an autoimmune neuromuscular disorder that disrupts communication at the neuromuscular junction. And today, treatment isn’t just about managing symptoms-it’s about stopping the attack before it starts.
How Myasthenia Gravis Actually Works
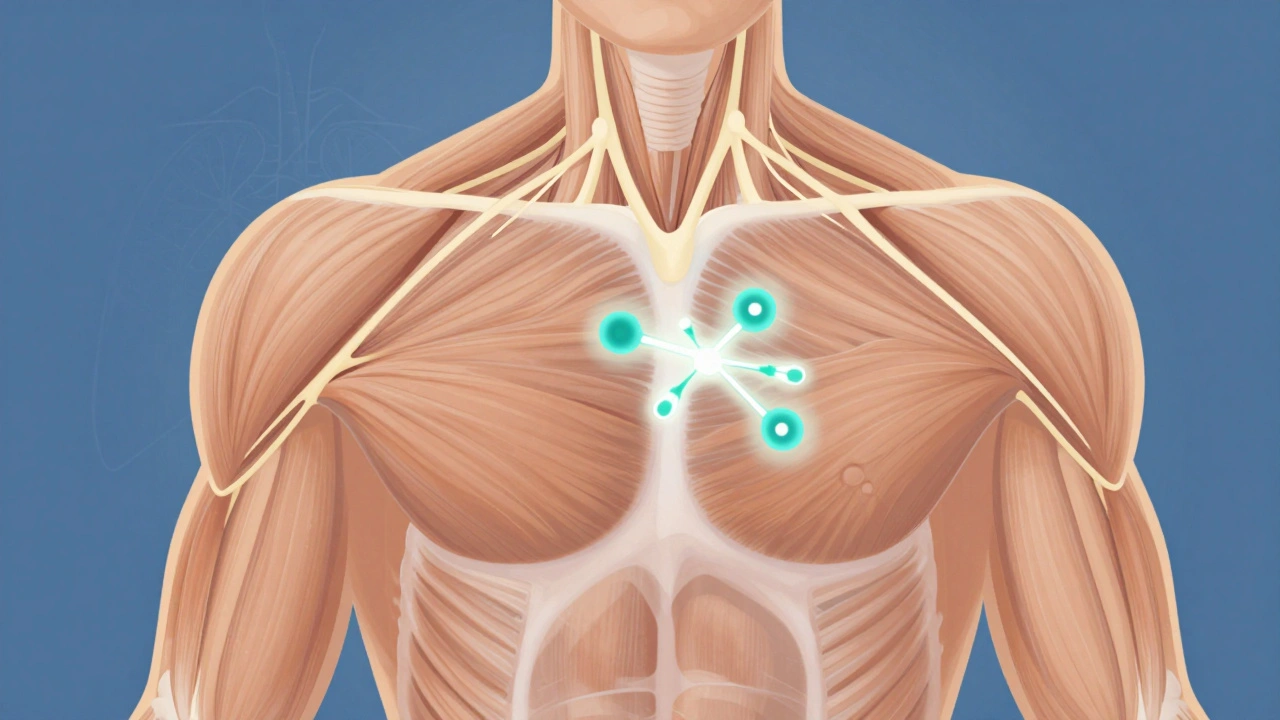
Your muscles move because nerves send signals through a chemical called acetylcholine. At the neuromuscular junction, acetylcholine binds to receptors on muscle cells, telling them to contract. In MG, your immune system makes antibodies that block or destroy those receptors. About 85% of people with generalized MG have antibodies against the acetylcholine receptor (AChR). Another 5-8% have antibodies against MuSK, a protein that helps organize those receptors. The rest-5-10%-are seronegative: no known antibody is detected, but the disease still happens.This isn’t a mystery from decades ago. In 1973, Patrick and Lindstrom proved these antibodies were the cause. That discovery changed everything. No longer was MG seen as an unexplained weakness-it was an autoimmune disease. And that meant treatment could target the immune system, not just the symptoms.
First-Line Treatments: Symptom Control and Immune Suppression
Most patients start with pyridostigmine (Mestinon), an acetylcholinesterase inhibitor. It doesn’t fix the root problem, but it slows down the breakdown of acetylcholine, giving more of it time to bind to the remaining receptors. Doses range from 60 to 120 mg every 3 to 6 hours. About 35-45% of people get stomach cramps, nausea, or diarrhea from it-but for many, it’s the difference between being able to eat and not.Then comes prednisone. This corticosteroid suppresses the immune system broadly. Doctors typically start at 0.5 to 1 mg per kg of body weight daily. Around 70-80% of patients see improvement within weeks. But the cost is high: weight gain in 65%, bone loss in 25% after one year, and new-onset diabetes in 15-20%. That’s why doctors don’t keep patients on high doses forever. The goal is to taper down as soon as possible.
That’s where chronic immunosuppressants come in. Azathioprine, mycophenolate, and cyclosporine are the mainstays. Azathioprine works in 60-70% of cases, but it takes 6 to 18 months to kick in. Mycophenolate is faster-65-75% response-and often preferred because it’s easier to tolerate. Cyclosporine hits 90% effectiveness but brings high blood pressure in 30% and kidney damage in 25%. These aren’t quick fixes. They’re long-term shields against immune attacks.
Thymectomy: Removing the Source of the Problem
The thymus gland, tucked behind the breastbone, plays a key role in immune development. In MG, especially in AChR-positive patients under 65, it’s often abnormal-enlarged or containing tumors called thymomas. The 2016 MGTX trial changed everything. Patients who had their thymus removed (thymectomy) had 56% less steroid use and 67% fewer hospitalizations over three years compared to those on steroids alone.Today, guidelines recommend thymectomy within 6 to 12 months of diagnosis for AChR-positive patients aged 18 to 65. The surgery can be done through a sternotomy (open chest), or minimally invasive methods like video-assisted thoracoscopic surgery (VATS) or robotic systems. Long-term data shows 35-40% of patients achieve complete stable remission five years after surgery-compared to just 15-20% with medication alone. But recovery isn’t easy. Fatigue lingers for many. And while minimally invasive techniques are less painful, their long-term outcomes are still being studied.
Fast-Acting Therapies: When You Need Immediate Help
There are times when MG flares up fast-when swallowing becomes dangerous, when breathing grows shallow. That’s when you need rapid intervention. Plasmapheresis and IVIG are the two go-to options.Plasmapheresis filters your blood, removing the bad antibodies. Five sessions over 7 to 10 days can clear 60-80% of them. Results show up in days. But the relief lasts only weeks. It’s not a cure-it’s a bridge.
IVIG (intravenous immunoglobulin) works differently. You get a concentrated dose of healthy antibodies from donors. These flood your system and confuse your immune cells, temporarily shutting down the attack. Dosed at 2 grams per kilogram over 2 to 5 days, it works just as fast as plasmapheresis. But it’s more expensive and harder to access in rural areas. Both are used for myasthenic crises-when you’re hospitalized because your breathing muscles are failing.
The New Wave: Targeted Biologics That Change Everything
The biggest shift in MG treatment happened after 2017, with the arrival of five FDA-approved biologics. These drugs don’t just suppress your whole immune system-they target specific parts of the attack.Complement inhibitors like eculizumab and ravulizumab block the final step of immune destruction at the neuromuscular junction. Eculizumab, given weekly then every two weeks, improves muscle strength significantly. In trials, 57% of patients reached minimal manifestation status-meaning almost no symptoms. But there’s a catch: you must get vaccinated against meningococcus first. These drugs carry a risk of deadly meningitis. Annual cost? $500,000-$600,000.
FcRn inhibitors are the game-changers. Drugs like efgartigimod, rozanolixizumab, nipocalimab, and batoclimab work by blocking the FcRn receptor-the protein that keeps harmful IgG antibodies alive in your body. Without it, antibodies break down fast. Within 1-2 weeks, IgG levels drop by 60-80%. You feel better fast. Rozanolixizumab is given as a weekly shot under the skin. Efgartigimod is an IV infusion. Nipocalimab, approved in April 2025 for teens and adults, reduces IgG by 70-80%. And batoclimab, with phase 3 results published in early 2025, matches efgartigimod’s results with less frequent dosing.
These drugs work across antibody types-even in seronegative MG. The ADAPT SERON study in 2024 showed 68% of seronegative patients responded to efgartigimod versus 30% on placebo. That’s huge. For years, seronegative patients had few options. Now they have real hope.
Rituximab, a B-cell therapy, is another option. It wipes out the immune cells that make the bad antibodies. It’s especially effective in MuSK-MG-80% respond. But in AChR-MG, only 50-60% benefit. It takes 8-16 weeks to work. Cost? $10,000-$15,000 per course. Still, for patients who don’t respond to other drugs, it’s a lifeline.
Real-World Challenges: Cost, Access, and Side Effects
The science is advancing. But real life isn’t so simple.Insurance hurdles are brutal. One Reddit user spent six months fighting for eculizumab approval. Another said they had to choose between paying for meds and rent. In the U.S., 40% of eligible patients can’t get these drugs because insurers deny coverage. Even when approved, prior authorization takes months.
Side effects matter too. Cyclosporine causes excessive hair growth and high blood pressure-so many patients quit. Long-term prednisone wrecks quality of life: mood swings, insomnia, weight gain, brittle bones. A 2024 MGFA study found 55% of patients on chronic steroids reported severe quality-of-life impairment. Only 25% on biologics did.
Patients are speaking up. On Myasthenia Gravis Foundation forums, 78% of 1,250 respondents said FcRn inhibitors improved their lives. Many prefer rozanolixizumab’s subcutaneous shots over IV infusions-even though 45% get injection site reactions. Convenience matters.

What Comes Next: The Future of MG Treatment
The next five years will bring even more change. Researchers are testing IgG4-specific biomarkers that may predict flare-ups before symptoms appear. Phase 2 trials of agrin mimetics (like AB1003) are showing promise in protecting the neuromuscular junction from damage. For older patients-30% of MG cases are over 65-new protocols are being designed to handle heart disease, kidney issues, and frailty alongside MG.And then there’s CAR T-cell therapy. Memorial Sloan Kettering launched a phase 1 trial in 2025 targeting B-cell maturation antigen. Early results? 60% of refractory patients went into remission at six months. It’s early, but if it holds, this could be a cure-not just control.
By 2028, 78% of neurologists believe treatment will be guided by antibody profiles and genetic markers. No more trial and error. Just precision medicine.
How Treatment Is Chosen Today
There’s no one-size-fits-all. Treatment depends on three things: antibody status, severity, and age.- Mild cases: Pyridostigmine alone or with low-dose prednisone.
- Generalized, moderate to severe: Pyridostigmine + prednisone + azathioprine or mycophenolate. Thymectomy if eligible.
- Severe or refractory: Biologics-FcRn inhibitors first for speed and broad use, complement inhibitors if AChR-positive and life-threatening.
- MuSK-positive: Rituximab is often second-line after steroids.
- Seronegative: FcRn inhibitors are now first-choice biologics.
Monitoring is key. Doctors track progress using MG-ADL (Myasthenia Gravis Activities of Daily Living) and QMG (Quantitative Myasthenia Gravis) scores every 4 to 12 weeks. Antibody levels don’t change fast enough to guide treatment-symptoms do.
Support Is Part of the Treatment
You don’t have to do this alone. The Myasthenia Gravis Foundation of America offers a 24/7 nurse hotline (answered within 3 minutes 95% of the time) and 147 local support groups. Talking to others who get it-someone who knows what it’s like to drop a coffee cup because your hand gives out-makes a difference. Therapy, mental health support, and pacing your day aren’t extras. They’re essential.Can myasthenia gravis be cured?
There is no universal cure yet, but many patients achieve long-term remission. About 35-40% of those who have thymectomy remain in stable remission after five years. Some patients on biologics or immunosuppressants reach minimal manifestation status-meaning they have almost no symptoms and don’t need daily medication. CAR T-cell therapy in early trials has shown remission in refractory cases, suggesting a potential path to cure in the future.
How long does it take for myasthenia gravis treatments to work?
It varies. Pyridostigmine works within 30 minutes but lasts only a few hours. Steroids like prednisone show improvement in 2-4 weeks. Traditional immunosuppressants like azathioprine take 6-18 months. FcRn inhibitors like efgartigimod or rozanolixizumab start working in 1-2 weeks. Complement inhibitors take 2-3 months. Rituximab takes 8-16 weeks. Timing matters when choosing therapy based on urgency.
Are biologics safe for long-term use?
Current data shows FcRn inhibitors are well tolerated over years. Long-term studies (up to 3 years) show sustained improvement without major safety signals. Complement inhibitors require lifelong meningococcal vaccination and carry a small but serious risk of meningitis. Rituximab can cause low immunoglobulin levels, increasing infection risk. All biologics are monitored closely with blood tests and symptom tracking. The benefit usually outweighs the risk in moderate to severe MG.
Can I get pregnant if I have myasthenia gravis?
Yes, but it requires careful planning. MG can worsen during pregnancy, especially in the first trimester and postpartum. Some drugs like mycophenolate and rituximab are unsafe during pregnancy. FcRn inhibitors are not yet proven safe for fetal use-pregnancy testing is required before starting them. Prednisone and pyridostigmine are generally considered safe. Work with a neurologist and high-risk OB-GYN before conceiving. Many women have healthy pregnancies with proper management.
What happens if I stop my medication?
Stopping medication without medical supervision can trigger a myasthenic crisis-a life-threatening worsening of muscle weakness, especially in breathing muscles. Even patients in remission should never stop drugs abruptly. Tapering must be slow and monitored. Some patients who achieve sustained remission (2+ years without symptoms or meds) may be able to stop under strict supervision, but relapse rates are high without continued immune control.
How do I know if my treatment is working?
Your doctor will use standardized scores like MG-ADL (daily activities) and QMG (clinical muscle strength) every 4-12 weeks. These are more sensitive than antibody levels, which change slowly. You’ll also track your own symptoms: Can you climb stairs without stopping? Can you hold your head up? Can you swallow without choking? Improvement in these areas means the treatment is working-even if lab results haven’t changed yet.
Is myasthenia gravis genetic?
MG is not directly inherited like cystic fibrosis or Huntington’s. But certain genes may increase your risk. People with HLA-B8 or DR3 genes are more likely to develop MG. Family members of MG patients have a slightly higher chance of autoimmune diseases-but not necessarily MG itself. It’s considered an autoimmune condition triggered by environmental factors (like viruses or stress) in genetically susceptible people.
Can lifestyle changes help manage myasthenia gravis?
Yes. Avoid overheating-heat makes weakness worse. Pace your activities. Rest before meals if swallowing is hard. Eat soft, easy-to-chew foods. Avoid statins, quinolone antibiotics, and beta-blockers-they can worsen MG. Regular, gentle exercise like walking or swimming helps maintain muscle tone without overexertion. Stress management matters too-flare-ups often follow emotional or physical stress.
Myasthenia gravis is no longer a sentence of decline. It’s a manageable condition-with more tools than ever before. The goal isn’t just survival. It’s living-fully, safely, without fear of the next muscle failing.




Myasthenia gravis isn’t just a medical condition-it’s a daily negotiation with your own body. I’ve watched friends go from hiking trails to needing help to lift a coffee cup, and the emotional toll is as real as the muscle fatigue. What’s remarkable is how far we’ve come: from guessing at causes to targeting specific antibodies like precision tools. The FcRn inhibitors? They’re not just science-they’re dignity restored.
It’s not about curing. It’s about reclaiming the quiet moments: a child’s laugh, a walk without stopping, the ability to swallow without fear. That’s the real victory.
And yes, the cost is obscene. But so is letting someone suffer because their insurance won’t blink.
Let’s not just celebrate the science-let’s fight for the people it’s meant to serve.
So I had a friend on efgartigimod-six weeks in, she finally held her grandson without her arms shaking. She cried. Not because she was ‘better’-but because she could *hold* him. That’s the thing no trial statistic captures. It’s not about numbers-it’s about the weight of a small hand in yours.
And yeah, the IV infusions suck. But if you’ve ever had to choose between breathing and paying rent, you’ll take the IV any day.
Also-seronegative folks? You’re not invisible anymore. That 68% response rate? That’s hope written in lab reports.
so like… biologics cost half a million a year??? and you’re telling me this isn’t just a pharma scam? like, who even gets this?? the 1%? i mean, i get it’s science but also… why does my asthma inhaler cost $300 and this costs a house??
also why is everyone acting like this is new? my uncle had MG in the 90s and they were already doing plasmapheresis. we just have better marketing now.
Just want to say-this is one of the clearest, most compassionate overviews of MG I’ve ever read. Not just the science, but the human stuff too. The part about pacing your day? That’s gold. You don’t need to push through. Rest isn’t weakness. It’s strategy.
And for anyone feeling alone-this community? It’s real. You’re not broken. You’re adapting. And that’s brave.
As someone from India, I’ve seen MG patients here struggle with access even more. Steroids are available, but biologics? Nearly impossible. Insurance doesn’t cover them, and out-of-pocket is a dream. We need global equity in treatment-not just innovation for the wealthy.
Also, thymectomy is underutilized here. Many doctors still treat it as ‘just fatigue.’ The 2016 MGTX trial should be mandatory reading in every med school in Asia.
Let’s not forget: science without access is just a luxury.
i’ve been on mycophenolate for 14 months. it took forever. i cried the first time i could open a jar without help. no one talks about how slow it is. everyone’s like ‘oh biologics are magic’-but what about the rest of us stuck in the waiting game?
also, prednisone gave me insomnia so bad i started sleeping in the bathtub. i’m not joking.
thank you for writing this. i felt seen.
Let me be blunt-this whole ‘precision medicine’ narrative is a distraction. The real issue? The U.S. healthcare system is a broken, profit-driven machine that turns life-saving drugs into commodities. Eculizumab costs $600K? That’s not science-it’s corporate extortion. We’re not curing disease-we’re monetizing suffering.
And don’t get me started on the ‘vaccination requirement’ for complement inhibitors. That’s not safety-it’s a bureaucratic chokehold to limit access. Who decided you need a meningitis shot to live? The FDA? The drug companies? The insurance CEOs?
Meanwhile, in countries with universal healthcare, patients get these drugs without begging. We don’t need better science-we need a revolution in how we value human life.
And for the record: if you think CAR T-cell therapy is ‘a cure,’ you’re ignoring the fact that it’s still experimental, toxic, and financially inaccessible. Hope isn’t a marketing slogan. It’s a right.
Wait-so the thymus is the problem? And they just cut it out? But didn’t the government say the thymus is part of the ‘immune control system’? And now they’re removing it… and giving us biologics that ‘confuse’ the immune system?
Isn’t this just… government experimentation? Who’s funding these trials? Big Pharma? The WHO? Are they tracking us through our antibodies now?
I read somewhere that MG is linked to 5G exposure. And now they’re selling us expensive infusions? Coincidence? I think not.
Also-why do all the studies say ‘seronegative’? Are they hiding the real cause? What if the antibodies aren’t the enemy? What if it’s the vaccines? Or the water? Or the… microwaves?
Just saying… something’s off.
Let’s be real. This isn’t medicine. It’s a spectacle. Biologics? $600K a year? That’s not treatment-that’s a billionaire’s charity project.
And the way people act like FcRn inhibitors are ‘miracles’? Please. It’s just another drug that makes you feel better for a few weeks before you’re back to square one. You think you’re cured? You’re just on a treadmill.
Meanwhile, the real heroes? The ones who show up to chemo with a playlist and a snack. The ones who still laugh when they drop their fork. That’s not in any trial. That’s real life.
And the doctors? They’re just playing God with a clipboard.
Stop glorifying the system. Start glorifying the people surviving it.
While the scientific advancements are laudable, the ethical implications of deploying these therapies without equitable global access are profoundly troubling. The disparity between the American patient who receives rozanolixizumab weekly and the Indian patient who cannot access pyridostigmine is not merely a logistical failure-it is a moral catastrophe.
Furthermore, the reliance on FcRn inhibitors, while clinically efficacious, constitutes a pharmacological Band-Aid that defers systemic reform. The root issue-autoimmune dysregulation-is being managed, not understood.
One must also interrogate the commercialization of patient vulnerability. The pharmaceutical industry’s marketing of biologics as ‘transformative’ obscures the fact that these are not cures, but expensive maintenance protocols.
And yet, we applaud the science while ignoring the suffering of those who cannot afford to participate in it. This is not progress. This is privilege masquerading as innovation.
ok but like… what if the real problem isn’t the antibodies… what if it’s the *stress*? i mean, my cousin got MG after her divorce. and her mom had lupus. and her dad had MS. so… is it genes? trauma? or… are we just all just too tired?
also, why is everyone so obsessed with ‘remission’? what if we just… accepted that our bodies are weird and we just learn to live with it? like, why do we need to ‘cure’ it? why can’t we just be okay with being fragile?
also-i think the thymus is a myth. they just cut it out because they didn’t know what else to do. like, remember when they used to cut out tonsils for everything?
and why do you think the drug companies are so quiet about the side effects? they don’t want you to know you might grow a beard from cyclosporine 😂
just saying… maybe we’re overcomplicating it.
I think the most beautiful part of this isn’t the drugs-it’s the shift in how we see patients. We used to treat MG as a failure of the body. Now we’re seeing it as a signal from the immune system that something’s out of balance.
That’s a huge philosophical change. It moves us from fighting our bodies to listening to them.
And maybe that’s the real breakthrough: not the biologics, but the humility to admit we don’t have all the answers-and that’s okay.
What if healing isn’t about erasing weakness… but learning to carry it with grace?
Let’s be honest here-the entire narrative around MG treatment is a construct. The FDA approvals? The clinical trials? The ‘minimal manifestation status’ metrics? All of it is designed to sell a product, not cure a disease. They’ve turned a neurological condition into a market segment. FcRn inhibitors? That’s not science-it’s a revenue stream with a side of hope.
And the patients? They’re not people anymore. They’re cohorts. They’re data points. They’re ‘responders’ and ‘non-responders.’
Meanwhile, the real cost-the sleepless nights, the canceled plans, the shame of needing help to stand up-is never measured in any trial.
And yet we’re told to be grateful for the ‘progress.’
Progress for whom?
Not for the uninsured. Not for the undocumented. Not for the ones who can’t afford to miss work for an infusion.
So don’t call this medicine. Call it capitalism with a stethoscope.
so i just found out my neurologist is on the board of a biologic company and now i’m wondering if my whole treatment plan was just a sales pitch… like i’m not even mad, i’m just… curious if my body is a product now
While your skepticism regarding commercialization is not unfounded, it inadvertently undermines the lived reality of patients who have regained function through these therapies. To dismiss biologics as mere profit-driven tools is to erase the dignity restored to those who can now hold their grandchildren, breathe without assistance, or speak without fear. The system is flawed-but so too is the notion that progress must be pure to be valuable. The goal is not perfection. It is presence. And for many, these drugs make presence possible.