When a doctor prescribes Baycip, you’re getting a brand‑name version of ciprofloxacin, a fluoroquinolone used for a range of bacterial infections. But it’s not the only game in town - several other antibiotics can do the job, sometimes with fewer side‑effects or a simpler dosing schedule. This guide breaks down Baycip, explains how it works, and compares it side‑by‑side with the most common alternatives so you can understand when each is appropriate.
Key Takeaways
- Baycip (ciprofloxacin) is a broad‑spectrum fluoroquinolone effective against many Gram‑negative bacteria.
- Levofloxacin and moxifloxacin are newer fluoroquinolones with better activity against certain respiratory pathogens.
- Azithromycin and doxycycline offer macrolide and tetracycline options, useful for atypical infections and when fluoroquinolones are contraindicated.
- Amoxicillin remains a first‑line choice for many common infections due to its safety profile and low cost.
- Choosing the right antibiotic depends on infection type, resistance patterns, patient health, and potential side‑effects.
What Is Baycip?
Baycip is a brand‑name tablet of ciprofloxacin, a fluoroquinolone antibiotic that inhibits bacterial DNA gyrase and topoisomerase IV, preventing DNA replication. In South Africa, Baycip is commonly prescribed for urinary tract infections (UTIs), gastrointestinal infections, and certain skin infections. Its standard adult dosage is 250mg to 500mg taken twice daily for 3‑14days, depending on infection severity.
How Ciprofloxacin Works
Ciprofloxacin targets the bacterial enzymes DNA gyrase (topoisomeraseII) and topoisomeraseIV. By binding to these enzymes, it creates double‑strand DNA breaks, halting bacterial cell division. This mechanism gives ciprofloxacin strong activity against many Gram‑negative organisms like Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa. However, its activity against Gram‑positive bacteria is more limited, which is why doctors often pair it with another drug for mixed infections.
When Baycip Is Usually Prescribed
Typical indications include:
- Uncomplicated urinary tract infections
- Traveler’s diarrhea caused by Campylobacter or Shigella
- Acute exacerbations of chronic bronchitis (when Haemophilus influenzae is suspected)
- Bone and joint infections caused by susceptible organisms
Because fluoroquinolones carry a boxed warning for tendon rupture, CNS effects, and QT prolongation, they are avoided in pregnant women, children, and patients with a history of tendon disorders.
Common Alternatives to Baycip
The following antibiotics are frequently considered when ciprofloxacin isn’t ideal.
Levofloxacin is a later‑generation fluoroquinolone that offers better coverage against atypical respiratory pathogens such as Mycoplasma pneumoniae and Legionella pneumophila. Typical adult dose: 500mg once daily for 5‑7days.
Moxifloxacin belongs to the fourth‑generation fluoroquinolones, providing enhanced activity against anaerobes and Gram‑positive cocci. It’s often used for community‑acquired pneumonia. Standard dose: 400mg once daily for 7‑14days.
Azithromycin is a macrolide antibiotic that blocks bacterial protein synthesis by binding to the 50S ribosomal subunit. It’s favored for sexually transmitted infections and atypical pneumonia. A common regimen: 500mg on day1, then 250mg once daily for 4days.
Doxycycline is a tetracycline that inhibits the 30S ribosomal subunit, preventing protein translation. It’s effective against a broad range of organisms, including Lyme disease and some resistant skin infections. Typical dose: 100mg twice daily for 7‑14days.
Amoxicillin is a beta‑lactam penicillin that interferes with cell‑wall synthesis. It remains first‑line for ear, nose, throat infections, and many uncomplicated UTIs. Common dose: 500mg three times daily for 5‑10days.
Side‑Effect Profiles at a Glance
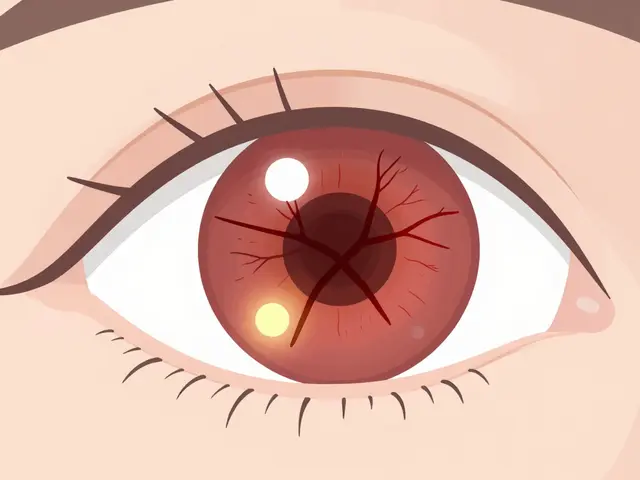
- Baycip (ciprofloxacin): Tendon pain/tendon rupture, photosensitivity, QT prolongation, nausea.
- Levofloxacin: Similar fluoroquinolone warnings, slightly lower risk of tendon issues, possible insomnia.
- Moxifloxacin: Higher risk of QT prolongation, especially in patients on other QT‑prolonging drugs.
- Azithromycin: GI upset, rare liver enzyme elevation, some QT lengthening.
- Doxycycline: Sunburn risk, esophageal irritation, mild GI upset.
- Amoxicillin: Generally well‑tolerated; occasional rash or diarrhea.
Comparison Table
| Brand (Generic) | Class | Typical Adult Dose | Primary Spectrum | Common Uses | Notable Side‑Effects |
|---|---|---|---|---|---|
| Baycip (Ciprofloxacin) | Fluoroquinolone | 500mg PO BID | Gram‑negative, some Gram‑positive | UTIs, GI infections, bone/joint | Tendon rupture, photosensitivity |
| Levofloxacin | Fluoroquinolone | 500mg PO QD | Broad, good for atypical respiratory | Pneumonia, sinusitis | Insomnia, modest tendon risk |
| Moxifloxacin | Fluoroquinolone (4th gen) | 400mg PO QD | Gram‑positive, anaerobes, atypical | Community‑acquired pneumonia | QT prolongation |
| Azithromycin | Macrolide | 500mg PO day1, then 250mg QD ×4 | Atypical, some Gram‑negative | STIs, atypical pneumonia | GI upset, rare liver issues |
| Doxycycline | Tetracycline | 100mg PO BID | Broad, especially intracellular | Lyme disease, acne, respiratory | Photosensitivity, esophageal irritation |
| Amoxicillin | Beta‑lactam (Penicillin) | 500mg PO TID | Gram‑positive, some Gram‑negative | Otitis media, sinusitis, uncomplicated UTIs | Rash, diarrhea |
How to Choose the Right Antibiotic
Think of antibiotic selection as a decision tree. Start with the infection site and likely pathogen, then consider local resistance data, patient allergies, and safety concerns.
- Identify the organism (or most likely suspects). If a urine culture shows E.coli susceptible to fluoroquinolones, Baycip is a solid choice.
- Check contraindications. A 68‑year‑old with a history of tendon rupture should avoid fluoroquinolones - consider amoxicillin or doxycycline instead.
- Review drug interactions. Patients on warfarin or antiarrhythmics need extra monitoring with moxifloxacin because of QT effects.
- Factor in dosing convenience. A single daily dose of levofloxacin may improve adherence compared with twice‑daily Baycip.
- Cost and availability. Amoxicillin is inexpensive and widely stocked, while newer agents might be pricier.
When in doubt, culture and sensitivity testing provides the most reliable guidance.

Safety Checklist for Patients Starting Baycip
- Are you over 60years old? Discuss tendon‑rupture risk with your doctor.
- Do you take corticosteroids? Combined use raises tendon‑damage odds.
- Any history of heart rhythm problems? Ask about QT‑interval monitoring.
- Are you pregnant, planning pregnancy, or breastfeeding? Choose an alternative.
- Do you have kidney impairment? Dose adjustment may be required.
Practical Tips for Managing Side‑Effects
If you experience mild nausea, take Baycip with food and a full glass of water. For photosensitivity, avoid prolonged sun exposure and wear sunscreen with SPF30+. Should you notice sudden joint pain or swelling, stop the medication and seek medical attention immediately - it could signal tendon involvement.
Frequently Asked Questions
Can I use Baycip for a simple sore throat?
A sore throat is usually viral, so antibiotics like Baycip aren’t needed. If a bacterial cause like streptococcus is confirmed, amoxicillin is the preferred first‑line treatment.
How long does it take for Baycip to work?
Most patients notice symptom improvement within 48‑72hours. Complete the prescribed course even if you feel better to prevent resistance.
Is it safe to take Baycip with alcohol?
There’s no direct interaction, but alcohol can worsen stomach upset, which some patients already experience with ciprofloxacin.
Why might my doctor prescribe levofloxacin instead of Baycip?
Levofloxacin offers once‑daily dosing and better coverage of atypical respiratory bugs, making it convenient for pneumonia or sinus infections where ciprofloxacin’s spectrum is less ideal.
Can I switch from Baycip to amoxicillin midway through treatment?
Only if a culture shows the infection is caused by an organism sensitive to amoxicillin. Changing antibiotics without confirmation can reduce effectiveness and promote resistance.
Next Steps for Readers
1. Review the comparison table and identify which antibiotic aligns with your infection type.
2. Check any personal risk factors (age, heart conditions, pregnancy).
3. Discuss the options with your healthcare provider, mentioning specific concerns like tendon health or QT prolongation.
4. If prescribed Baycip, follow the safety checklist and report any unusual pain promptly.
5. Keep a copy of this guide in your medicine cabinet for quick reference.
Choosing the right antibiotic isn’t just about effectiveness; it’s also about safety and tolerability. By weighing the pros and cons of Baycip against its alternatives, you can make an informed decision that supports a swift recovery and minimizes unwanted side‑effects.






When considering an antibiotic, it is essential to match the drug’s spectrum with the likely pathogen and the patient’s risk factors. Baycip (ciprofloxacin) offers strong Gram‑negative coverage but carries warnings such as tendon rupture and QT prolongation. For uncomplicated urinary tract infections in a healthy adult, it remains a reasonable first‑line option if culture data support susceptibility. However, in older patients or those with a history of tendon disorders, alternatives like amoxicillin or doxycycline may provide a safer profile. Always discuss the side‑effect profile and dosing convenience with your clinician before initiating therapy.
The therapeutic index of fluoroquinolones, particularly ciprofloxacin, is subject to pharmacokinetic‑pharmacodynamic optimisation, yet the risk‑benefit calculus often skews unfavourably in geriatric cohorts. One could argue the marginal efficacy gain does not justify the elevated incidence of collagen‑related adverse events.
Sure, because tossing a high‑potency fluoroquinolone at every infection is exactly the nuanced approach modern medicine prides itself on.
Wow!!! This guide is super helpful!!! I love how it breaks down each drug’s pros and cons – makes picking the right one a breeze!!! Just remember to finish the full course, even if you feel better, to avoid resistance!!
It is incumbent upon the prescribing clinician to conduct a rigorous differential diagnosis, integrating local antibiogram data and patient‑specific contraindications; only then may the selection of Baycip versus levofloxacin be deemed scientifically justified. 📊
Great summary! I’d add that discussing any recent antibiotic use with your doctor can help avoid unnecessary resistance buildup, and checking for drug‑drug interactions, especially with anticoagulants, is always wise.
Choosing an antibiotic is, in many ways, a microcosm of ethical decision‑making: we balance efficacy against potential harm, consider the broader ecological impact, and remain mindful of the individual’s lived experience. Let this guide serve as a compass, not a prescription, as you navigate those choices.
Remember, side‑effects can sneak up-stay vigilant!!
Our country's hospitals have abundant generic amoxicillin; relying on expensive brand‑name fluoroquinolones like Baycip is a misallocation of resources 😒.
Reading through the comparison, one cannot help but notice the intricate interplay of pharmacodynamics, patient comorbidities, and health‑system economics that underlie each therapeutic choice. While Baycip boasts a robust Gram‑negative spectrum, its propensity for tendon toxicity and QT prolongation casts a long shadow over its otherwise appealing efficacy. In contrast, levofloxacin offers the convenience of once‑daily dosing, which may improve adherence among patients who struggle with complex regimens, yet it does not escape the class‑wide warnings attached to fluoroquinolones. Moxifloxacin, as a fourth‑generation agent, expands coverage to anaerobes and certain Gram‑positive organisms, making it a valuable tool in community‑acquired pneumonia, but the heightened risk of cardiac arrhythmias demands meticulous cardiac monitoring. Azithromycin, beloved for its anti‑inflammatory properties, provides a macrolide alternative with a relatively benign side‑effect profile, although emerging resistance among Streptococcus pneumoniae threatens its future utility. Doxycycline’s broad intracellular activity renders it indispensable for atypical infections, yet photosensitivity remains a practical concern for patients with outdoor occupations. Amoxicillin’s time‑tested safety and low cost solidify its position as a first‑line staple, but rising β‑lactamase production has eroded its effectiveness in certain regions. The decision matrix, therefore, should commence with an accurate identification of the causative organism, whether through culture or reliable clinical judgment, before layering in patient‑specific factors such as age, renal function, and concomitant medications. For a 70‑year‑old individual with a prior Achilles tendon rupture, the prudent path steers away from fluoroquinolones entirely, favoring alternatives like doxycycline or amoxicillin where appropriate. Conversely, in a young adult presenting with a multidrug‑resistant Pseudomonas urinary tract infection, Baycip may indeed be the optimal choice, provided close monitoring is instituted. Cost considerations cannot be ignored; while brand‑name ciprofloxacin may strain a patient’s budget, many health systems negotiate lower prices or offer generic equivalents that maintain therapeutic parity. Ultimately, the clinician must weigh the nuanced benefits against the tangible risks, communicate these trade‑offs transparently, and empower the patient to participate actively in the treatment plan. By doing so, we honor both the science of antimicrobial stewardship and the art of patient‑centered care.