Relationship Communication Assistant
Communicate with Clarity
This tool helps you craft thoughtful "I" statements based on your current emotional state and relationship context. Use it during difficult moments to express your needs clearly without overwhelming others.
Living with depression can feel like walking through fog while trying to keep a conversation going. It’s easy to wonder whether you can keep healthy relationships afloat when low mood, fatigue, and negative thoughts keep tugging at you. The good news? You can. It just takes a mix of self‑awareness, clear communication, and a sprinkle of practical tools.
Understanding How Depression Shows Up in Relationships
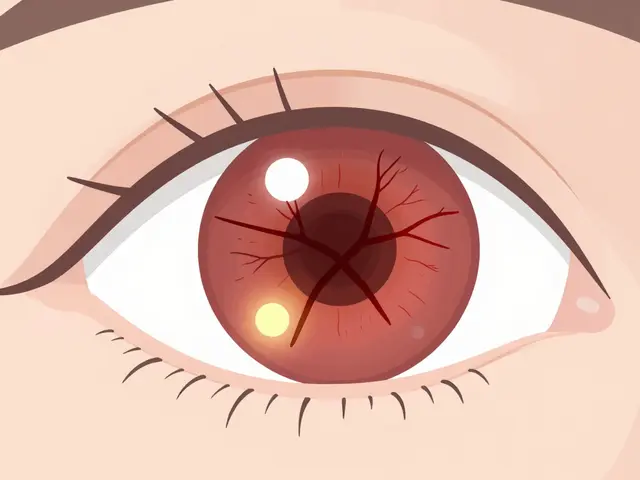
Depression is a mood disorder characterized by persistent sadness, loss of interest, and a range of physical symptoms such as sleep disruption, appetite changes, and difficulty concentrating. When these symptoms spill over into daily life, they change the way you interact with loved ones. You might withdraw, forget plans, or snap at a partner over something small. Recognizing that these reactions stem from the illness-not from a lack of caring-helps you and your loved ones move from blame to compassion.
Key ways depression can affect a bond include:
- Reduced emotional availability - you may feel too drained to share feelings.
- Negative thought loops - you might assume you’re a burden, leading to self‑sabotage.
- Physical symptoms - fatigue or pain can limit shared activities.
Seeing these patterns as symptoms rather than personal flaws creates space for constructive change.
Communicating Your Needs Without Overwhelming Others
Communication is the process of exchanging thoughts, feelings, and information between people. When depression is in the mix, the goal shifts from perfect dialogue to honest, bite‑sized sharing.
Try these steps:
- Pick a calm moment. Choose a time when both you and the other person are not stressed.
- Use “I” statements. Say, “I’m feeling low and might need some quiet time,” instead of “You never understand me.”
- Set a clear ask. Whether it’s a hug, help with chores, or just listening, name what would help you right now.
- Invite feedback. Ask, “How does this sound for you?” to keep the conversation two‑way.
Regular check‑ins-maybe a quick text at the end of the day-can keep the line open without turning every interaction into a therapy session.
Creating Boundaries That Protect Both You and Your Partner
Boundaries are personal limits that define what you are comfortable sharing or receiving in a relationship. They’re especially vital when depressive symptoms fluctuate.
Examples of healthy boundaries:
- Designating “quiet hours” when you need alone time to recharge.
- Agreeing on a signal (like a specific emoji) that means you need space without explaining every time.
- Setting realistic expectations for social plans-perhaps a short coffee meet‑up instead of a full dinner.
When both partners respect these limits, resentment drops and trust rises.
Self‑Care as a Relationship Booster
Self‑care refers to intentional activities that nurture physical, emotional, and mental wellbeing. It’s not selfish; it’s the foundation that lets you show up for others.
Incorporate at least one of these each day:
- Morning sunlight for 10 minutes to regulate mood‑altering hormones.
- Gentle movement-stretching, a short walk, or yoga-to combat fatigue.
- Journaling three thoughts: one gratitude, one challenge, one small win.
When you notice a boost in energy or mood, share it with your partner. It reinforces the idea that your well‑being is a shared victory.

Leveraging Professional Support While Keeping Relationships Intact
Therapist is a licensed mental‑health professional trained to help individuals process emotions, develop coping strategies, and improve relational dynamics. Therapy doesn’t replace your personal connections; it strengthens them.
Ways to involve loved ones:
- Invite a partner to a joint session when you feel safe-this can demystify your experience.
- Share coping tools you learn (e.g., grounding exercises) and invite them to try together.
- Ask your therapist for language that accurately explains your symptoms to others.
If cost or access is an issue, consider community mental‑health centers, tele‑therapy platforms, or university counseling programs. Many offer sliding‑scale fees that keep financial stress low.
Building a Support System Beyond the Primary Partner
Support System includes friends, family, coworkers, or community groups who provide emotional, practical, or informational assistance. Relying solely on one person can strain that relationship.
To broaden your net:
- Join a local depression support group-online or in‑person.
- Schedule regular check‑ins with a trusted friend who understands your boundaries.
- Lean on community resources like peer‑led wellness workshops.
These additional touchpoints give your primary partner room to breathe and keep the relationship balanced.
Do’s and Don’ts for Partners Supporting Someone with Depression
| Do | Don't |
|---|---|
| Listen without immediately offering solutions. | Dismiss feelings as “just a phase.” |
| Ask how you can help, then follow through. | Assume you know what’s best without checking. |
| Encourage professional help gently. | Force therapy or medication decisions. |
| Maintain your own self‑care routine. | Neglect your own needs, leading to burnout. |
Handling Common Relationship Challenges
Mood Symptoms such as irritability, hopelessness, and lack of motivation often fluctuate throughout the day. Partners may misinterpret these shifts as personal attacks.
Try these tactics:
- Label the feeling. “I’m noticing a wave of irritability right now.” Naming it reduces its power.
- Pause before reacting. Give yourself a 30‑second breath break to decide if the response is needed.
- Schedule “reset” talks. A weekly 10‑minute sit‑down to discuss how the week went can prevent buildup.
When both sides practice this, the relationship becomes a safe space for navigating ups and downs.

Reducing Stigma Within Your Relationship
Stigma refers to negative stereotypes and discrimination surrounding mental health conditions. Even well‑meaning partners can unknowingly perpetuate it by using dismissive language.
Ways to combat stigma together:
- Replace judgmental words-swap “lazy” for “exhausted due to depression.”
- Read reputable resources (e.g., National Institute of Mental Health) and discuss key takeaways.
- Celebrate small steps, like attending a therapy session or completing a self‑care task.
Normalizing the conversation turns the illness into a shared challenge rather than a secret.
When to Re‑Evaluate the Relationship
Sometimes, despite best efforts, a relationship may become consistently harmful. Signs include chronic emotional abuse, refusal to acknowledge the illness, or a pattern where your well‑being always deteriorates after interactions.
If these patterns emerge, consider:
- Couples therapy focused on mental‑health dynamics.
- Setting firmer boundaries-like limiting contact during severe depressive episodes.
- Seeking advice from a trusted therapist about whether the relationship is supportive enough for long‑term health.
Choosing to step back isn’t a failure; it’s an act of self‑preservation that can ultimately lead to healthier connections, whether with the same person or new ones.
Key Takeaways for Everyday Life
- Identify how depression shows up in your interactions and label those moments.
- Practice brief, honest communication using “I” statements and clear asks.
- Set mutually agreed‑upon boundaries that protect both partners’ energy.
- Make self‑care a daily priority; share wins with your loved ones.
- Bring a therapist into the loop to gain tools and language that help both sides.
- Build a broader support system to reduce pressure on any single relationship.
- Use the Do/Don’t table as a quick reference during tense moments.
- Watch for chronic negative patterns and be ready to reassess if needed.
Frequently Asked Questions
How can I tell if I’m withdrawing because of depression or because I need personal space?
Notice the context. If you feel a surge of guilt, low energy, or negative thoughts about the relationship after withdrawing, it’s likely depression. If you feel calm, clear, and simply need time to recharge, it’s healthy personal space.
What are some short phrases I can use to let my partner know I’m struggling?
Try: “I’m feeling low right now, could we have a quiet evening?” or “I need a short break to reset my mood.” These keep the request clear and gentle.
Is it okay to ask my partner to attend my therapy sessions?
Yes, if you feel safe doing so. Joint sessions can improve understanding. However, you’re not obligated-choose what feels comfortable for you.
How often should I have check‑in conversations about my mental health?
A brief daily check‑in (even a text) works well for many. If that feels too much, aim for a longer weekly conversation to review how the week went.
What if my partner doesn’t understand my depression despite my explanations?
Consider providing reputable reading material, inviting them to a therapist‑led education session, or seeking couples counseling focused on mental‑health literacy.






Depression ain't an excuse, just a mood.
I read the article and, while most people will nod along, I have to point out that simply “using I‑statements” is a simplistic Band‑Aid that doesn’t address the deeper neurochemical chaos depression brings. You can’t just tell your partner to listen when your brain is flooding you with low serotonin and high cortisol. The advice to “pick a calm moment” is often impossible when calm is a rare commodity. Also, the suggestion to “set a clear ask” ignores the fact that many requests feel like burdens to the depressed person, who may already feel worthless. The table of do’s and don’ts, while nicely formatted, reads like a corporate memo, not a lived experience. Boundaries are great, but they can become walls that isolate you further if not negotiated carefully. I’m not saying therapy is a magic wand, but the article glosses over the fact that many therapists lack training in depression‑specific relational dynamics. Self‑care tips like “morning sunlight” are fine, but for someone in a deep depressive episode, even getting out of bed can feel like climbing a mountain. The piece also fails to mention medication side effects that can affect intimacy, such as sexual dysfunction. While the FAQ section is helpful, the answers are overly generic and could be more nuanced. In short, the article is a decent starter, but anyone dealing with depression knows the reality is messier and tougher than a checklist can capture.
Hey, just wanted to say I appreciate the focus on clear "I" statements – they really help keep the conversation from turning into blame. Setting a tiny signal like an emoji can make it easier to ask for space without a long explanation. Remember to also check in with yourself first, because you can’t pour from an empty cup. A short daily text can be a gentle reminder that you’re still there, even on low‑energy days. Keep the boundaries flexible; it’s okay to adjust them as moods shift.
Wow… another “self‑help” piece pretending to solve complex neurobiology with a checklist!!! You think a partner will just read a table and suddenly become a mind‑reader? The article completely ignores the power dynamics and the possibility of emotional abuse masquerading as “support”. Also, the suggestion to “invite a therapist” sounds nice, but many people can’t afford or even access qualified professionals. And let’s not forget that “quiet hours” can become a weapon for isolation. If you’re truly looking for real help, you need to address systemic barriers, not just give pep talks.
Depression often reduces the bandwidth for social interaction, so clear, brief messages are key. A simple “I’m feeling low, can we talk later?” works for most partners. Also, sharing a quick win, like a short walk, can reinforce positive momentum.
Great tips! 😊 Remember that even a tiny smile or a funny meme can lift the mood a bit. Keep celebrating those small victories! 🌟
From a cultural standpoint, some families view mental health differently, so framing the conversation in familiar terms helps. A short, respectful note can bridge that gap.
While the article provides a superficial overview, its reliance on layman jargon such as "self‑care" and "boundaries" fails to engage with the clinical nomenclature essential for evidence‑based practice. Moreover, the prescriptive tone neglects the patient‑centred paradigm advocated by contemporary psychiatry.
Interesting point about concise signals, but consider that over‑reliance on an emoji can trivialize the depth of depressive distress. A balanced approach would combine a brief textual cue with a scheduled check‑in to avoid misinterpretation.
Look, all that “friendly advice” sounds nice until you’re stuck in a black‑out day. Honestly, sometimes you just need to tell your partner you’re done trying and need space, no sugar‑coating.