When someone is diagnosed with celiac disease, the focus usually turns to gut symptoms: bloating, diarrhea, weight loss. But what many don’t realize is that liver abnormalities are one of the most common extra-intestinal signs - often showing up before digestive issues do. In fact, up to 40% of untreated celiac patients have abnormal liver enzyme levels, yet most doctors don’t test for celiac when they see a fatty liver or elevated ALT. That’s a missed opportunity.
Why Does Celiac Disease Affect the Liver?
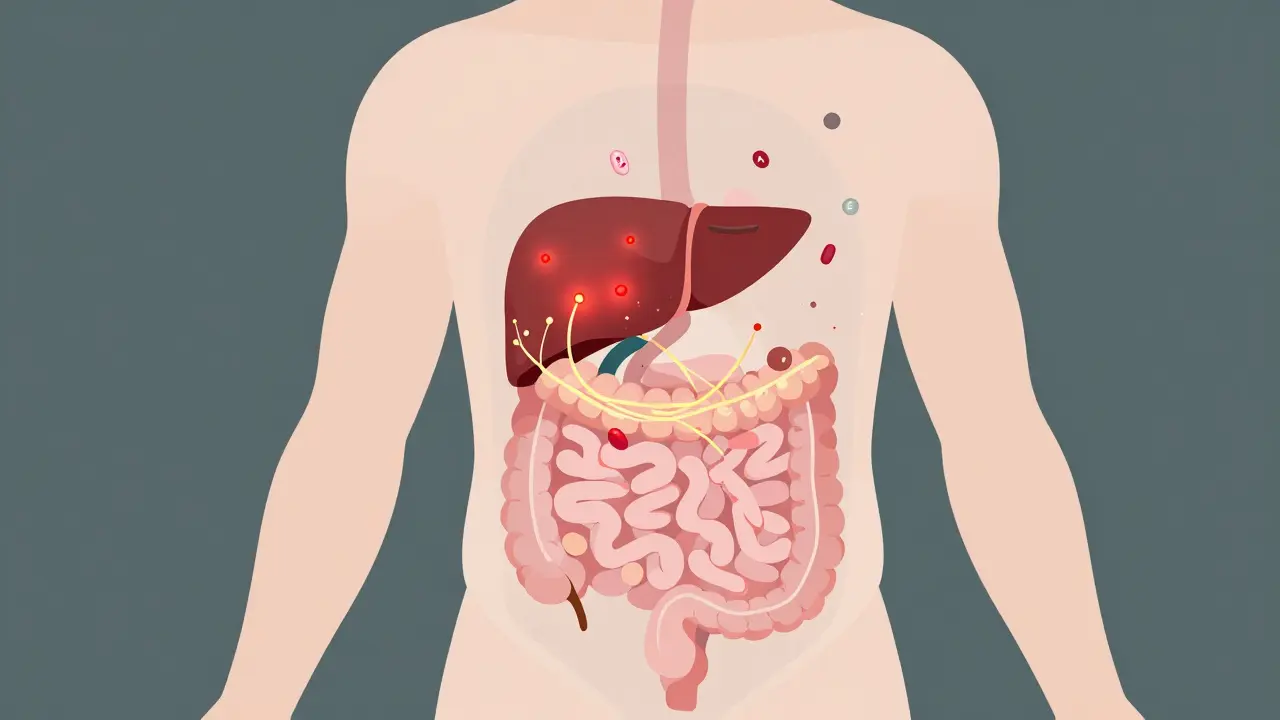
Celiac disease isn’t just about the small intestine. It’s an autoimmune condition where the body attacks its own tissues after gluten exposure. That immune chaos doesn’t stop at the gut. The liver, being the body’s main filter, gets caught in the crossfire. Three main mechanisms link celiac to liver problems.First, a leaky gut. When gluten damages the intestinal lining, toxins and undigested food particles slip into the bloodstream. The liver has to process them. Over time, that constant bombardment triggers inflammation. Second, autoimmune cross-reactivity. The immune system, already on high alert from gluten, sometimes mistakes liver cells for foreign invaders - leading to conditions like autoimmune hepatitis. Third, malabsorption. Celiac patients often lack fat-soluble vitamins like A, D, E, and K. These vitamins help protect the liver. Without them, the organ becomes more vulnerable to damage.
The most common sign? Elevated liver enzymes. ALT and AST levels rise in about 37% of celiac patients at diagnosis. That’s nearly double the rate seen in people without celiac. What’s surprising is how mild these elevations usually are - often just 2 to 5 times the upper limit of normal. That’s not enough to alarm most doctors, who might assume it’s just fatty liver or alcohol use. But in celiac patients, it’s often the first red flag.
What Liver Conditions Are Linked to Celiac Disease?
Celiac disease doesn’t just cause vague enzyme spikes. It’s tied to specific liver diseases:- Non-alcoholic fatty liver disease (now called MASLD): About 25-50% of celiac patients show fat buildup in the liver on biopsy. But here’s the twist - it’s not always from being overweight. Malabsorption and inflammation play a bigger role than diet alone.
- Autoimmune hepatitis: Up to 6.4% of people with autoimmune hepatitis also have celiac disease. And vice versa - 4-6.4% of celiac patients develop autoimmune hepatitis. This isn’t coincidence. Shared genetic markers like HLA-DQ2 make you prone to both.
- Primary biliary cholangitis and primary sclerosing cholangitis: These rare bile duct diseases are more common in celiac patients than in the general population.
- Cryptogenic cirrhosis: One in 20 people with unexplained cirrhosis turns out to have undiagnosed celiac disease. That’s why some guidelines now recommend celiac screening for anyone with unexplained liver scarring.
What’s striking is how reversible this is. In 79% of cases, liver enzymes return to normal within 12 to 18 months of starting a strict gluten-free diet. Biopsies show reduced inflammation and even reversal of early fibrosis. That’s rare in other liver diseases. Viral hepatitis needs antivirals. Alcoholic liver disease requires quitting alcohol. But for celiac, the fix is simple - remove gluten.
The Gluten-Free Diet Paradox
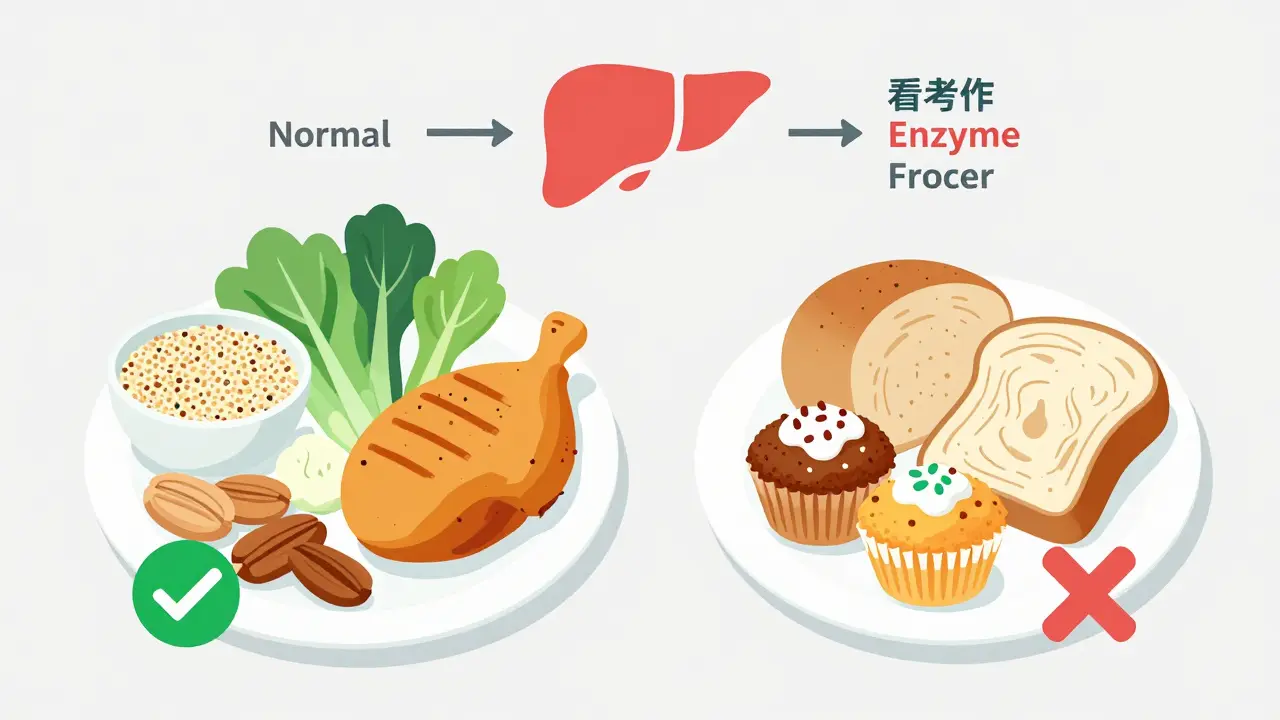
Here’s where things get tricky. A gluten-free diet heals the gut - but it can hurt the liver if done wrong.Many gluten-free products are loaded with refined carbs, sugar, and unhealthy fats to mimic the texture of wheat. A gluten-free muffin isn’t healthier - it’s just wheat-free. For someone with celiac, switching to these processed foods can lead to weight gain, insulin resistance, and ultimately, MASLD. A 2023 study found that celiac patients who ate mostly processed gluten-free foods had a 3.5 times higher risk of developing fatty liver than those who ate whole foods like vegetables, lean meats, legumes, and naturally gluten-free grains like quinoa and buckwheat.
That’s why nutritional guidance matters. Patients who work with a dietitian who specializes in celiac disease normalize their liver enzymes 30% faster than those who just get a generic gluten-free list. The key is balance: avoid gluten, but don’t replace it with junk. Focus on fiber-rich foods, healthy fats from nuts and fish, and protein sources like eggs, chicken, and beans.
How Is It Diagnosed?
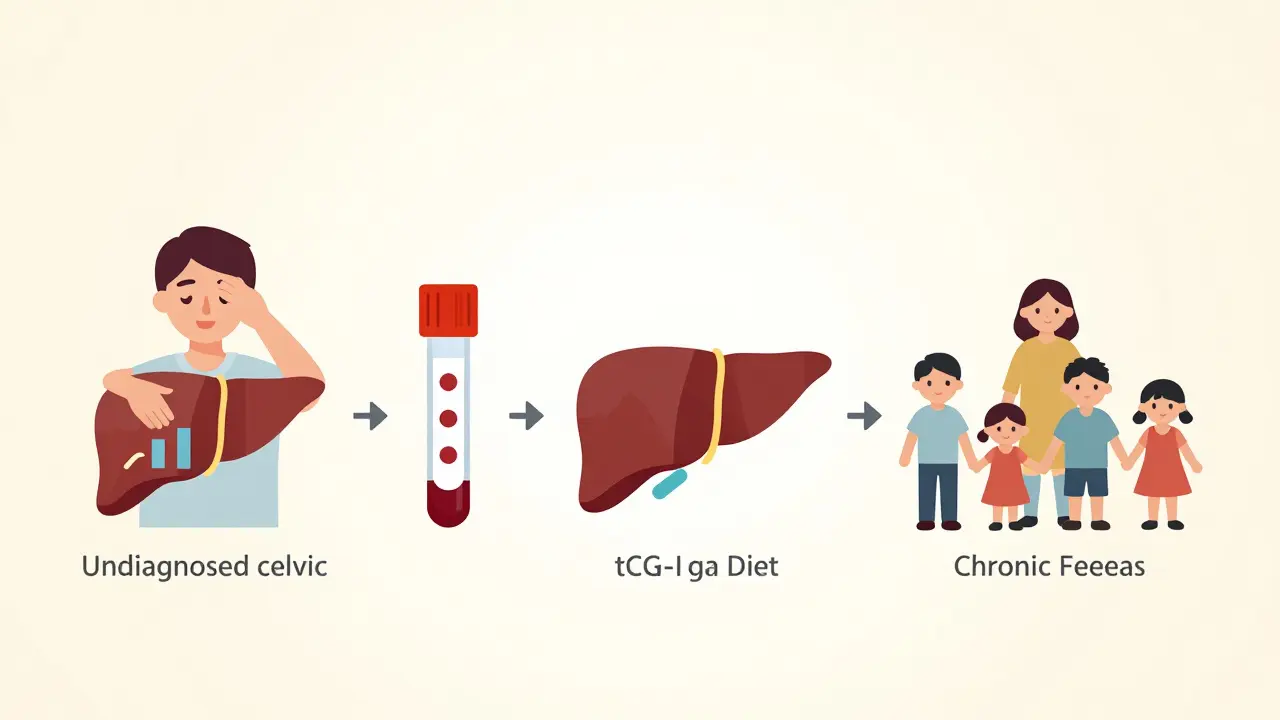
If you have unexplained elevated liver enzymes - especially if you’ve had digestive issues, fatigue, or unexplained anemia - get tested for celiac disease. The standard test is a blood panel for tTG-IgA antibodies. But here’s the catch: if you’ve already started a gluten-free diet, the test can be falsely negative. Always test before eliminating gluten.Doctors now screen for celiac more often than before. In 2024, 92% of clinics included liver enzyme tests in their initial celiac workup - up from just 65% in 2015. If your ALT or AST is high and you have no history of alcohol use, viral hepatitis, or obesity, celiac should be on the list. A simple blood test can change everything.
For patients with persistent liver enzyme abnormalities after 12 months on a gluten-free diet, further testing is needed. Autoimmune hepatitis, primary biliary cholangitis, or even undiagnosed MASLD from poor diet may be the culprit. A liver biopsy isn’t always needed, but it’s the gold standard if enzymes stay high.
What Happens After Diagnosis?
The good news? Most people see big improvements. In a 2015 study by Dr. Daniel Leffler, 79.3% of celiac patients with abnormal liver enzymes saw them return to normal within 1.5 years of going gluten-free. For many, fatigue fades, nausea disappears, and blood work looks clean.But timing matters. The longer you go untreated, the higher the risk of lasting damage. One 2025 study found that siblings with celiac disease had twice the rate of chronic liver disease compared to their unaffected brothers and sisters. Early diagnosis isn’t just about digestion - it’s about protecting your liver for life.
Monitoring is key. Get liver enzymes checked at diagnosis, then every 3-6 months until they normalize. After that, annual checks are enough - unless symptoms return. And if you’re struggling with the gluten-free diet, find a specialist. A dietitian who knows celiac can help you avoid the hidden traps that lead to fatty liver, nutrient deficiencies, and inflammation.
What’s Next in Research?
Scientists are digging deeper. Researchers at the University of Helsinki are tracking 500 celiac patients over 10 years to see if the length of gluten exposure before diagnosis predicts liver damage. Early data suggests the longer you eat gluten unknowingly, the higher your risk of fibrosis.Another focus: genetics. People who carry two copies of the HLA-DQ2 gene (homozygous) are 2.3 times more likely to develop liver abnormalities than those with just one copy. That could lead to targeted screening - testing not just everyone with high enzymes, but those with high-risk genes too.
Pharmaceutical companies are also stepping in. Takeda’s Phase II trial, completed in late 2023, tested an enzyme therapy that breaks down gluten in the gut before it triggers an immune response. If it works, it could reduce liver inflammation in people who accidentally ingest gluten - a game-changer for those who struggle with cross-contamination.
And guidelines are changing. The European Association for the Study of the Liver now recommends screening all patients with cryptogenic cirrhosis for celiac disease. That’s huge. It means doctors are finally connecting the dots.
Bottom Line: Don’t Ignore the Liver
Celiac disease is more than a gluten intolerance. It’s a systemic autoimmune disorder - and the liver is one of its most common targets. Elevated liver enzymes aren’t always about alcohol, obesity, or poor lifestyle. Sometimes, they’re your body screaming that you have celiac disease.If you’ve been told you have fatty liver but don’t fit the typical profile - no obesity, no diabetes, no drinking - get tested for celiac. If you’ve been diagnosed with celiac and your liver enzymes are still high after a year on a gluten-free diet, don’t assume it’s hopeless. Look for coexisting conditions. Talk to a specialist. Reassess your diet.
The liver is resilient. With the right diet and early action, most of the damage can be undone. You don’t need pills. You don’t need surgery. You just need to stop eating gluten - and eat well while you do it.
Can celiac disease cause elevated liver enzymes even without digestive symptoms?
Yes. Up to 40% of people with celiac disease have elevated liver enzymes without noticeable gut problems. Fatigue, joint pain, or unexplained anemia may be the only signs. Liver enzyme abnormalities can actually be the first clue that someone has celiac disease.
Will my liver enzymes return to normal on a gluten-free diet?
In about 79% of cases, yes - within 12 to 18 months of strict gluten avoidance. The liver has a strong ability to heal itself once the trigger (gluten) is removed. Biopsies often show reduced inflammation and even reversal of early scarring.
Can a gluten-free diet cause fatty liver?
Yes - if you replace gluten-containing foods with processed gluten-free products high in sugar, refined carbs, and unhealthy fats. Many packaged gluten-free snacks, breads, and pastas are nutritionally poor. A diet based on whole foods - vegetables, lean proteins, nuts, legumes, and naturally gluten-free grains like quinoa - reduces the risk of developing MASLD.
Should I get tested for celiac if I have unexplained fatty liver?
If you have fatty liver without typical risk factors like obesity, diabetes, or heavy alcohol use, celiac disease should be ruled out. Up to 4.7% of people with cryptogenic cirrhosis have undiagnosed celiac. A simple blood test for tTG-IgA antibodies can identify it - but only if you’re still eating gluten.
How often should liver enzymes be checked after a celiac diagnosis?
Check at diagnosis, then every 3-6 months until levels normalize - usually within 12 months. After that, annual monitoring is sufficient unless symptoms return or enzymes rise again. Persistent elevation after a year may indicate coexisting liver disease like autoimmune hepatitis.
Is there a genetic link between celiac disease and liver problems?
Yes. People with two copies of the HLA-DQ2 gene (homozygous) are 2.3 times more likely to develop liver abnormalities than those with one copy. This gene also increases risk for autoimmune hepatitis and other immune-related conditions, explaining why celiac and liver disease often occur together.





Man, I never realized celiac could mess with your liver like that. I got diagnosed last year after my ALT was sky-high and I didn’t even have stomach issues. Just constant fatigue and joint aches. Doc thought it was stress. Turns out, gluten was wrecking my liver. Went gluten-free and my enzymes dropped in 4 months. No meds, no surgery. Just stop eating the poison.
This is such an important post. So many people are told they have fatty liver and told to lose weight or cut out alcohol, but no one checks for celiac. I’ve seen patients in my clinic with normal BMI and zero alcohol use who had massive enzyme spikes-turned out they had silent celiac. Early testing saves lives.
Love how this breaks it down. I’m a nutrition coach and I’ve had so many clients come to me after being told their liver is ‘failing’-only to find out gluten was the culprit. But here’s the kicker: half of them switched to gluten-free junk food and got fatter. The diet matters. Real food > gluten-free cookies.
My cousin was diagnosed with cryptogenic cirrhosis at 38. No alcohol, no obesity. They finally tested for celiac after 3 years of dead ends. Turned out she’d had it since she was 12. Her liver improved so much after going gluten-free. Why isn’t this standard?
Just had my first liver panel in 2 years. ALT was normal. Been gluten-free for 18 months. No more brain fog. No more random nausea. I didn’t even know how bad it was until it was gone. This post nailed it. Eat real food. Avoid the fake gluten-free crap. Your liver will thank you.
There is a well-documented association between celiac disease and autoimmune liver conditions, particularly autoimmune hepatitis and primary biliary cholangitis, with shared HLA haplotypes conferring increased susceptibility. The mechanism involves molecular mimicry and increased intestinal permeability leading to systemic immune activation. It is imperative that hepatologists incorporate serological screening for celiac disease in patients with unexplained transaminitis, particularly when other etiologies have been excluded.
Gluten isn’t just a ‘tummy thing’-it’s a full-body arsonist. 🔥 Your liver? It’s the firefighter working overtime while the whole house burns. And guess what? Most docs don’t even carry a hose. They just hand you a pamphlet on ‘eating better’ while your enzymes scream for help. Cut the gluten. Eat real food. Stop letting Big Gluten fool you.
Why do Americans make everything so complicated? In India, we know gluten is poison. If your liver is bad, stop eating wheat. No blood tests needed. No fancy studies. Just stop. Simple.
Everyone’s talking about gluten-free but nobody talks about how hard it is to find real food. I tried the diet but everything I ate was sugar and oil. My liver didn’t improve. My mood crashed. I felt worse. Maybe it’s not the gluten, maybe it’s the fake food they sell you.
Just read this after my biopsy showed early fibrosis. My doc said ‘maybe celiac?’ and I laughed. I had no symptoms. But I got tested anyway. Positive. Went gluten-free. 6 months later, fibrosis markers dropped. Still eating gluten-free junk, though. Maybe I need to stop buying those ‘healthy’ gluten-free granola bars. 😅