Chronic diarrhea that won’t go away-no blood, no fever, no obvious cause-can be one of the most frustrating health problems to live with. For many people, especially those over 50, this isn’t just an inconvenience. It’s a life disrupted: constant bathroom trips, sleepless nights, social isolation, and the fear that something serious is wrong. The culprit? Microscopic colitis. It’s not visible on a colonoscopy. No one can see it with their eyes. But under a microscope, the damage is clear. And there’s a treatment that works-budesonide-that’s changed the game for thousands.
What Exactly Is Microscopic Colitis?
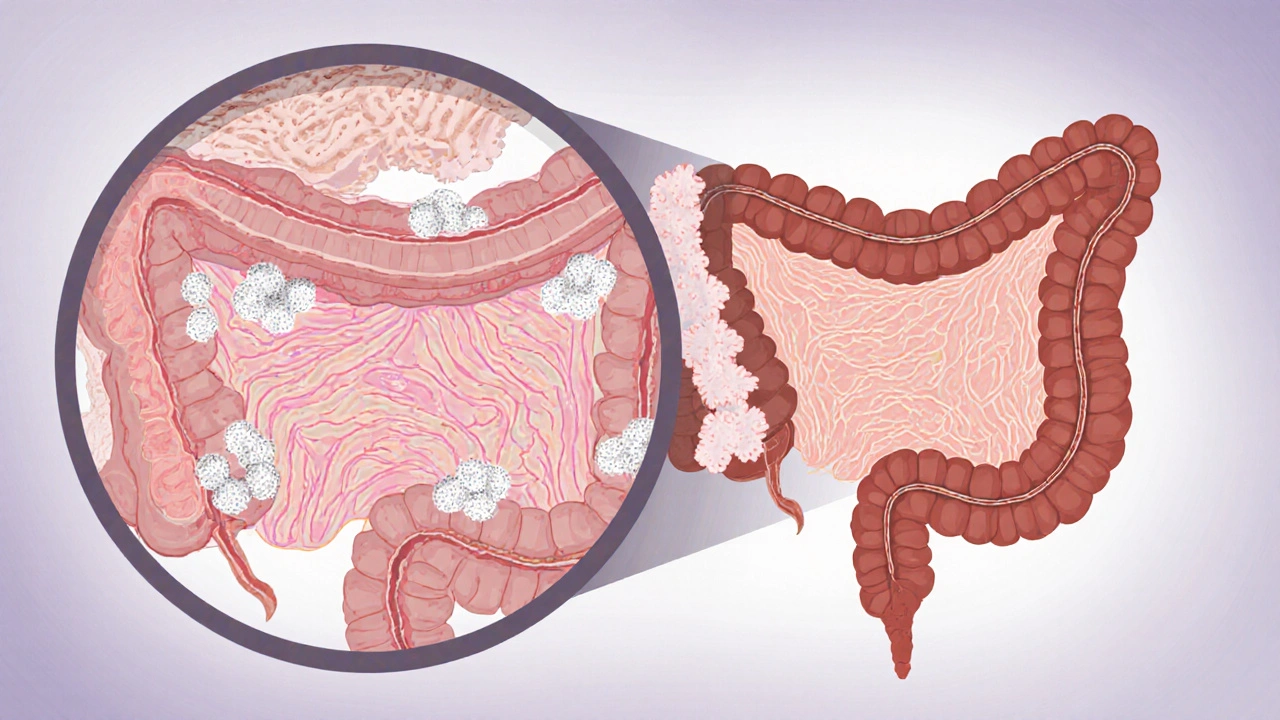
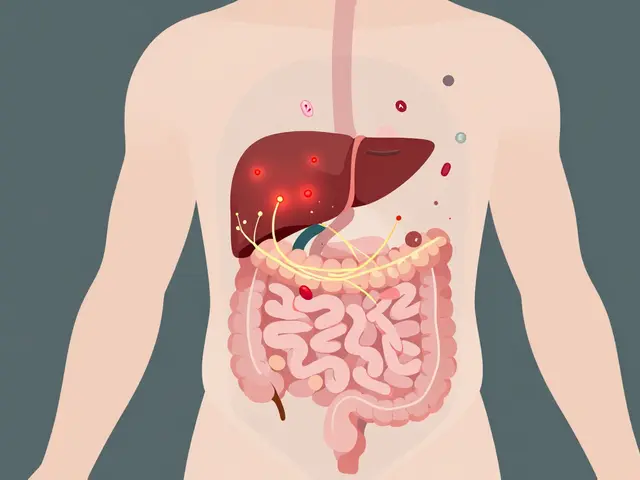
Microscopic colitis isn’t one disease. It’s two: collagenous colitis and lymphocytic colitis. Both cause the same symptoms-frequent, watery diarrhea, often 5 to 10 times a day-and both look completely normal during a colonoscopy. That’s why so many people go years without a diagnosis. Doctors check for Crohn’s, ulcerative colitis, infections, food intolerances. Nothing shows up. So they tell you it’s IBS. But it’s not. The real problem hides in the colon lining. In lymphocytic colitis, too many white blood cells (lymphocytes) pile up between the cells that line the gut. In collagenous colitis, a thick band of collagen-like scar tissue-forms just beneath the surface. Either way, the colon can’t absorb water properly. That’s why your stool is always liquid. It’s not a gut infection. It’s not food poisoning. It’s inflammation you can’t see unless you look at a tissue sample under a microscope. It’s more common than you think. About 5 out of every 100,000 people get it each year. Women are affected twice as often as men. Most cases show up between ages 55 and 70. And it doesn’t come and go quickly. People often suffer for months, sometimes years, before someone finally takes a biopsy and finds the answer.Why Budesonide Is the First-Line Treatment
Before budesonide, the go-to treatment was prednisone-a strong, full-body steroid. It worked, but it came with a price: weight gain, high blood sugar, mood swings, bone thinning, insomnia. For older adults, especially those already at risk for osteoporosis or diabetes, the side effects were often worse than the disease. Budesonide changed everything. It’s still a steroid, but it’s designed to work only where it’s needed-in the gut. About 90% of it gets broken down by the liver before it ever enters your bloodstream. That means very little circulates through your body. The result? High effectiveness with far fewer side effects. Clinical trials show that 75% to 85% of people with microscopic colitis go into remission within 6 to 8 weeks of taking 9 mg of budesonide daily. That’s compared to only 25% to 30% on a placebo. In one major study, 84% of collagenous colitis patients had their diarrhea stop completely after 8 weeks on budesonide. Only 38% did on sugar pills. It’s not magic. But it’s the closest thing we have.How Budesonide Works and What to Expect
Most people start feeling better within 10 to 14 days. Some report a dramatic drop in bathroom visits-from 10 times a day to 2 or 3. That’s not just relief. That’s a return to normal life. You can sleep through the night. You can leave the house without planning your route around bathrooms. You can stop carrying extra clothes. The standard dose is 9 mg once a day for 6 to 8 weeks. After that, your doctor will check your symptoms. If you’re in remission, they’ll slowly reduce the dose-usually by 3 mg every 2 to 4 weeks. Tapering too fast can cause a relapse. About half of people who stop budesonide completely will have symptoms come back within a year. That’s why many people need maintenance therapy. If your symptoms return after stopping, your doctor might put you on a lower daily dose-6 mg or even 3 mg-to keep things under control. For some, this means staying on budesonide for months or even years.
What Are the Side Effects?
Because budesonide stays mostly in the gut, side effects are mild compared to older steroids. But they’re not zero. The most common ones:- Insomnia (about 15% of users)
- Acne or skin changes (12%)
- Mood swings or irritability (8%)
- Headaches
- Minor bloating or nausea
What If Budesonide Doesn’t Work?
About 15% to 20% of people don’t respond to budesonide. That’s frustrating, but there are other options. Bismuth subsalicylate (Pepto-Bismol) helps about 26% of people. It’s cheap, available over the counter, and safe for short-term use. Some patients take it daily for months and find it keeps symptoms at bay. Mesalamine (Asacol, Lialda) is another option. It works for 40% to 50% of people. It’s often used if budesonide causes side effects or if someone prefers a non-steroid. For those with bile acid diarrhea-common in microscopic colitis-cholestyramine (Questran) can be a game-changer. It binds excess bile in the gut and stops diarrhea in up to 70% of cases. Many patients do better on a combo: budesonide plus cholestyramine. Anti-TNF drugs like infliximab? They’re expensive ($2,500 to $3,000 per infusion) and carry infection risks. They’re only considered if everything else fails.
The Cost and Accessibility Issue
Budesonide is available as a generic, which dropped the price significantly since 2018. A full 8-week course now costs $150 to $250 with insurance. Without insurance, it’s still cheaper than the branded version (Entocort EC), which can run $800 to $1,200. But cost isn’t just about the pills. Long-term users need monitoring: bone density scans every 1 to 2 years, blood tests for glucose and liver function. That adds $300 to $500 a year in out-of-pocket costs for some. Many patients on Reddit and patient forums say the biggest barrier isn’t the drug-it’s the lack of awareness. Too many doctors still think chronic diarrhea is IBS. Too many patients are told to “just manage it.” That’s why diagnosis takes an average of 11 months from first symptom to confirmed biopsy.What’s Next for Microscopic Colitis Treatment?
Research is moving fast. In 2023, the FDA gave fast-track status to vedolizumab, a biologic drug that targets gut-specific inflammation. Early results show 65% of patients in remission after 14 weeks. It’s not approved yet, but it could be the next big thing for people who don’t respond to budesonide. Scientists are also looking at genetics. Early data from the COLMICS trial suggests people with certain genes (HLA-DQ2/DQ8) respond better to budesonide. In the future, a simple blood test might tell you whether budesonide is right for you before you even start. For now, budesonide remains the gold standard. It’s the treatment endorsed by every major gastroenterology group in Europe and North America. It’s the one most doctors reach for first. And for good reason: it works, it’s safe, and it gives people their lives back.What You Can Do Now
If you’ve had unexplained watery diarrhea for more than 3 weeks:- Ask your doctor for a colonoscopy with biopsies-not just a visual exam, but tissue samples from the colon.
- Make sure the pathologist knows to look for microscopic colitis. Many labs don’t routinely check for it unless specifically asked.
- If diagnosed, don’t fear steroids. Budesonide is not prednisone. It’s targeted. It’s safe for short-term use.
- Track your symptoms. How many bowel movements a day? Any pain? Weight loss? Nighttime symptoms? This helps your doctor adjust your treatment.
- Consider combining treatments. If bile acid diarrhea is suspected, ask about cholestyramine.




After years of being told it's IBS, I finally got diagnosed with collagenous colitis last year. Budesonide was a miracle. I went from 12 runs a day to 2-3, and I slept through the night for the first time in 5 years. No more carrying extra pants. No more panic when I leave the house. It’s not perfect, but it’s the closest thing to normal I’ve had in a decade.
Thank you for writing this. I hope more doctors read it.
I’m still on budesonide after 18 months on 3mg daily. My doc says I’m one of the lucky ones who doesn’t relapse when tapering. But honestly? I’m not even trying to stop anymore. If this is what ‘maintenance’ looks like, I’ll take it. Better than living like a human toilet.
Also, cholestyramine saved me when the budesonide dose dropped too fast. Weird chalky taste, but worth it.
Ugh. Another post glorifying steroids like they’re some kind of magic potion. People don’t talk about how budesonide messes with your mood. I got so irritable I yelled at my cat for breathing too loud. And insomnia? Try sleeping when your brain is buzzing like a damn phone on vibrate.
And don’t even get me started on the ‘it’s safe’ nonsense. You’re telling me a steroid that suppresses your immune system is fine for long-term use? My grandma’s on it and now she’s got shingles. Coincidence? I think not.
My buddy took budesonide for 6 weeks and said it felt like his gut finally shut up. No more midnight dashes to the bathroom. He went from ‘can’t travel’ to ‘booked a road trip to Banff.’
But yeah, the cost is nuts if you’re uninsured. I had to help him find a patient assistance program. Pharma companies make bank on this stuff. Still, if it works? Worth it. Just wish more docs knew about it.
The reductionist framing of microscopic colitis as a ‘steroid-responsive condition’ obscures the broader pathophysiological context. The epithelial barrier dysfunction, coupled with aberrant T-cell infiltration and dysregulated mucosal immune homeostasis, suggests a multifactorial etiology that pharmacologic suppression merely mitigates.
Furthermore, the reliance on budesonide as a first-line agent reflects a therapeutic inertia rooted in clinical inertia rather than mechanistic superiority. The absence of biomarkers for patient stratification renders this approach empiric, not precision. The COLMICS trial’s HLA-DQ2/DQ8 correlation, while promising, remains underpowered and geographically skewed. Until we move beyond symptom suppression toward immune reprogramming, we are merely managing a symptom complex, not treating a disease.
Canada’s healthcare system is failing us. I had to wait 9 months just to get a biopsy. My doctor said ‘it’s probably IBS’ like I’m some hypochondriac. Then I paid $1,200 out of pocket for budesonide because my insurance ‘doesn’t cover experimental treatments.’
Meanwhile, Americans are getting biologics like vedolizumab and laughing all the way to the bank. Why do we have to beg for basic care? This isn’t science. This is a joke.
And yes, I’m taking Pepto-Bismol on top of it. Screw the side effects - I’d rather be alive than ‘properly medicated.’ 😤
THIS IS ALL A LIE. Budesonide is just a cover-up for the government’s secret bioweapon program. They put it in the water so we get chronic diarrhea and then they sell us the cure. The real cause? 5G towers + glyphosate + the WHO’s agenda. I’ve been tracking my bowel movements since 2018 and the spikes match every time they ‘update’ the CDC guidelines.
Also, your doctor is paid by Big Pharma. Don’t trust them. Go to the clinic in Mexico. They give you raw goat milk enemas. It’s cheaper and works better. I know. I’ve done it. I’m a veteran. I’ve seen the truth.
PS: Why does everyone say ‘microscopic colitis’? It’s not microscopic. It’s MAGA colitis. They’re hiding the truth from us.
As a gastroenterologist with 22 years in practice, I’ve seen the data. Budesonide is not a cure. It’s a Band-Aid. The real issue is gut microbiome dysbiosis. The fact that 50% relapse after discontinuation proves this. We need fecal transplants, not steroids. But insurance won’t cover it because it’s ‘experimental’ - even though the studies show 70% remission rates.
And the HLA-DQ2/DQ8 correlation? That’s not ‘promising.’ That’s the key. We’re ignoring genetic predisposition because it’s inconvenient. We treat symptoms, not causes. That’s medical malpractice by design.