Quick Takeaways
- Montair (montelukast) is a leukotriene receptor antagonist taken once daily.
- It works well for mild‑to‑moderate asthma and seasonal allergic rhinitis.
- Inhaled corticosteroids (ICS) like fluticasone are more potent for persistent asthma but need a device.
- Antihistamines such as loratadine are cheap for sneezing and itching but won’t control asthma.
- Choosing the right drug depends on severity, age, cost, and side‑effect tolerance.
Below is a straight‑forward look at Montair and the most common alternatives. The goal is to help you or your doctor decide which option fits your health situation best.
Montair vs alternatives
What is Montair (Montelukast)?
Montair is the brand name for montelukast, a leukotriene receptor antagonist (LTRA) approved for asthma maintenance and allergic rhinitis. It blocks leukotrienes - inflammatory molecules that cause airway narrowing and mucus production. By stopping these chemicals, Montair reduces nighttime cough, wheeze, and seasonal sniffles.
How Montair Works
Leukotrienes are released after exposure to allergens, cold air, or exercise. When they bind to receptors in the bronchial walls, they trigger smooth‑muscle contraction and swelling. Montair binds to the same receptors but does not activate them, essentially “turning off” the signal.
This oral tablet (10 mg for adults, 4 mg chewable for children 2‑5 yr, 5 mg for ages 6‑14 yr) reaches peak blood levels within 3‑4 hours and can be taken at any time of day. Because it works systemically, no inhaler is needed, which many patients find convenient.
When to Use Montair
- Mild‑to‑moderate persistent asthma as a controller medication.
- Exercise‑induced bronchoconstriction (EIB) when a quick‑acting inhaler isn’t practical.
- Seasonal or perennial allergic rhinitis (hay fever) in adults and children.
Guidelines from the Global Initiative for Asthma (GINA) place Montair as an add‑on for patients who cannot tolerate inhaled corticosteroids or need extra control for allergy symptoms.
Pros and Cons of Montair
Advantages
- Once‑daily oral dosing - easy for kids and busy adults.
- No mouth‑thrush risk that inhaled steroids carry.
- Effective for both asthma and allergic rhinitis in a single pill.
Potential Drawbacks
- Rare neuropsychiatric events (mood changes, insomnia, rare suicidality) - FDA boxed warning.
- Less potent than inhaled corticosteroids for moderate‑to‑severe asthma.
- Cost varies by brand; generic montelukast is cheaper but may not be available everywhere.
Common Alternatives
Below are the main drug families doctors consider when Montair isn’t ideal.
Inhaled corticosteroids (ICS) are the cornerstone of asthma control. They reduce airway inflammation directly at the source. Popular options include:
- Fluticasone propionate - a high‑potency spray used once or twice daily.
- Budesonide - another spray with a slightly lower dose requirement for children.
Antihistamines block histamine receptors and are excellent for sneezing, itchy eyes, and runny nose, but they do not address bronchoconstriction. Common over‑the‑counter choices are:
- Loratadine - non‑sedating, 10 mg once daily.
- Cetirizine - slightly more sedating, 10 mg once daily.
Omalizumab is a monoclonal antibody for severe allergic asthma that targets IgE. It is given as a subcutaneous injection every 2‑4 weeks and is reserved for patients who fail high‑dose ICS plus LABA.
Side‑by‑Side Comparison
| Drug | Class | Typical Dose | Primary Use | Onset of Action | Common Side Effects | Approx. Monthly Cost (US$) |
|---|---|---|---|---|---|---|
| Montair | Leukotriene receptor antagonist | 10 mg tablet daily | Asthma maintenance, allergic rhinitis | 3‑4 hours | Mood changes, abdominal pain, headache | ~$10‑$15 (generic $5‑$7) |
| Fluticasone propionate | Inhaled corticosteroid | 100‑250 µg inhalation 1‑2×/day | Persistent asthma control | 1‑2 weeks for full effect | Oral thrush, hoarseness, adrenal suppression | ~$30‑$45 |
| Budesonide | Inhaled corticosteroid | 200‑400 µg inhalation 1‑2×/day | Asthma, COPD | 1‑2 weeks | Thrush, cough, mild adrenal effects | ~$25‑$40 |
| Loratadine | Antihistamine | 10 mg tablet daily | Allergic rhinitis, urticaria | 30‑60 minutes | Headache, dry mouth | ~$5‑$10 |
| Cetirizine | Antihistamine | 10 mg tablet daily | Allergy symptoms | 30‑60 minutes | Sedation (15‑20% of users) | ~$5‑$12 |
| Omalizumab | Anti‑IgE monoclonal antibody | 150‑600 mg SC injection q2‑4 wks | Severe allergic asthma | Weeks to months (clinical response) | Injection site reaction, rare anaphylaxis | ~$1200‑$1500 |

How to Choose the Right Option
Ask yourself these questions before settling on a medication:
- What is the severity of my asthma? If it’s mild‑to‑moderate and I prefer a pill, Montair is a solid starter.
- Do I have trouble using an inhaler? Oral tablets avoid technique errors that many patients make.
- Am I also battling seasonal allergies? Montair covers both, while antihistamines only treat nasal symptoms.
- Is cost a major concern? Generic montelukast is cheap, but high‑dose inhaled steroids may be covered by insurance.
- Do I have a history of mood or psychiatric issues? If yes, discuss the neuropsychiatric warning with a doctor.
For persistent asthma that isn’t controlled with Montair alone, stepping up to an inhaled corticosteroid (or adding a long‑acting beta‑agonist) is the next logical move. In rare, severe cases, biologics like omalizumab become an option.
Key Takeaways for Patients and Caregivers
- Montair is convenient, works for both asthma and allergic rhinitis, and is safe for children over 2 years.
- It isn’t as strong as inhaled steroids for chronic airway inflammation.
- Antihistamines are cheap adjuncts for nasal symptoms but won’t protect lungs.
- Severe, uncontrolled asthma may need a combination of inhaled steroids, LABA, or biologic therapy.
- Always review side‑effect profiles with your clinician, especially the rare mood‑related alerts.
Frequently Asked Questions
Can I take Montair and an inhaler together?
Yes. Montair is often prescribed as an add‑on to inhaled corticosteroids when asthma isn’t fully controlled by the inhaler alone. The combination targets two different pathways - leukotrienes and inflammation.
Is Montair safe for pregnant women?
Pregnancy category B (US). Studies haven’t shown a clear risk, but doctors usually prefer inhaled steroids as the first line during pregnancy. Talk to your obstetrician before starting.
Why do some users report mood changes on Montair?
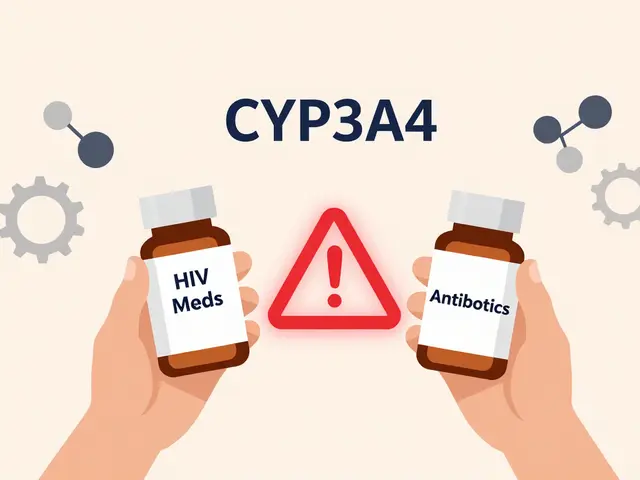
Montelukast can cross the blood‑brain barrier and affect neurotransmitter pathways in a small subset of people. If you notice anxiety, depression, or unusual thoughts, stop the drug and contact a healthcare professional immediately.
How quickly does Montair start working for exercise‑induced bronchoconstriction?
Peak plasma levels appear in 3‑4 hours, so most doctors advise taking the tablet at least 2 hours before vigorous activity.
Is a generic version of Montair as effective?
Generic montelukast contains the same active ingredient and has passed bio‑equivalence tests, so it works just as well. The main difference is price.




Montelukast represents a valuable tool in the therapeutic arsenal against asthma and allergic rhinitis. Its oral administration bypasses the technical challenges associated with inhaler devices. Patients often report greater adherence when a once‑daily pill replaces multiple inhalations. The drug’s mechanism of blocking leukotriene receptors directly addresses inflammatory pathways. Clinical trials have demonstrated a reduction in nighttime symptoms and rescue inhaler use. While inhaled corticosteroids remain the gold standard for severe disease, Montelukast offers a solid alternative for milder cases. The convenience factor cannot be overstated for busy professionals and caretakers alike. Moreover, the medication’s safety profile is favorable, with most adverse events limited to mild gastrointestinal upset. The rare neuropsychiatric warnings merit vigilance, but they should not eclipse the overall benefit. For individuals who struggle with inhaler technique, the oral route eliminates a common source of treatment failure. Health insurers frequently cover generic montelukast, which keeps out‑of‑pocket costs low. Pediatric patients as young as two years can safely receive the chewable formulation. Seasonal allergy sufferers also appreciate the dual‑action nature of the drug. In practice, many clinicians start with Montelukast before escalating to higher‑dose inhaled steroids. This step‑wise approach aligns with guideline recommendations and promotes personalized care. Ultimately, Montelukast empowers patients to manage their respiratory health with confidence and simplicity.
Big pharma hides cheaper Indian versions of montelukast behind a veil of brand loyalty.
India’s pharmaceutical industry has been producing high‑quality generic montelukast for decades, yet many patients remain unaware of its efficacy. The domestic version matches the reference product in bio‑equivalence and costs a fraction of the branded price. Choosing a reputable Indian manufacturer can therefore preserve therapeutic benefit while easing the financial burden. This option is especially relevant for families without comprehensive insurance coverage.
A quick tip for anyone starting Montelukast: take the tablet with food or a glass of milk to minimize stomach discomfort. If you’re switching from an inhaled corticosteroid, keep a short‑acting reliever on hand for breakthrough symptoms during the first two weeks. Monitoring mood changes is essential; inform your physician promptly if you notice anxiety or depressive thoughts. Lastly, remember that adherence drops dramatically when doses are missed, so set a daily reminder on your phone.
Good point Celeste, especially the food tip – I’ve had a few patients who felt less nausea after taking it with breakfast. Also, keeping the rescue inhaler handy during the transition is a smart move. I’d add that checking the pharmacy label for the correct chewable strength avoids dosing errors in kids.
Montelukast is a leukotriene receptor antagonist; its pharmacodynamics involve competitive inhibition at CysLT1 receptors. Bioavailability approximates 64% with a Tmax of 3‑4 h. The drug’s half‑life permits once‑daily dosing, optimizing patient compliance. Clinical efficacy is quantified by reductions in Asthma Control Questionnaire scores.
While the aforementioned overview extols the virtues of Montelukast, it neglects to address the potential for iatrogenic psychotropic disturbances in susceptible individuals, a nuance that cannot be dismissed as peripheral. Moreover, the economic argument presupposes uniform insurance formularies, an assumption that fails under scrutiny when considering regional reimbursement disparities. Consequently, a blanket endorsement of montelukast as a cost‑effective solution is, at best, an oversimplification of a multifaceted therapeutic landscape. A judicious clinician must therefore weigh these variables rather than adopt a monolithic prescribing paradigm.