Ever wondered why restless leg syndrome (RLS) runs in some families? The answer lies in a mix of genes, brain chemistry, and lifestyle factors. This article breaks down the latest research, shows which genes matter most, and offers practical steps if you suspect a hereditary link.
What Is Restless Leg Syndrome?
Restless Leg Syndrome is a neurological disorder characterized by uncomfortable sensations in the legs, often accompanied by an irresistible urge to move them. Symptoms typically flare at night, disrupting sleep and daily life. The International Restless Legs Study Group estimates that up to 10% of adults experience RLS symptoms at some point, with about 2% meeting clinical criteria for moderate to severe disease.
RLS is more than an annoyance; chronic sleep loss can increase the risk of hypertension, depression, and impaired glucose metabolism. Understanding why it occurs helps doctors target treatment and lets patients take preventive steps.
Why Genetics Matters in RLS
Family and twin studies have long hinted that RLS isn’t solely an environmental condition. A classic 2004 twin study reported a heritability estimate of 54%, meaning over half of the variation in RLS risk can be traced to genetic factors. More recent genome‑wide association studies (GWAS) have identified several DNA regions that consistently appear in people with RLS.
In plain language, if a parent has RLS, their children inherit a set of genetic variants that increase the odds of developing the disorder. However, genetics is just one piece of the puzzle; iron status, medication use, and lifestyle also play big roles.
Key Genes Linked to RLS
Since the first GWAS for RLS in 2007, researchers have pinpointed at least five robust risk genes. The table below summarizes the most replicated findings, the biological pathways they influence, and the frequency of the risk allele in European populations.
| Gene | Primary Function | Risk Allele (e.g., rsID) | Allele Frequency* | Key Study (Year) |
|---|---|---|---|---|
| MEIS1 homeobox transcription factor involved in neuronal development | Neuronal differentiation, iron regulation | rs12469063 | 0.28 | Schormair et al., 2017 |
| BTBD9 BTB domain protein linked to dopaminergic signaling | Dopamine pathway modulation | rs3923809 | 0.34 | Huang et al., 2008 |
| PNPLA3 lipid‑metabolism enzyme | Lipid handling, iron storage | rs738409 | 0.22 | Schormair et al., 2019 |
| NOS1 neuronal nitric oxide synthase | Neurotransmitter regulation | rs1057910 | 0.31 | Stefan et al., 2020 |
| PLXNA4 plexin A4 involved in axon guidance | Neural circuit formation | rs3738319 | 0.27 | Schormair et al., 2021 |
*Allele frequency reported for individuals of European ancestry; frequencies differ in Asian and African populations.

How These Genes Influence RLS Pathophysiology
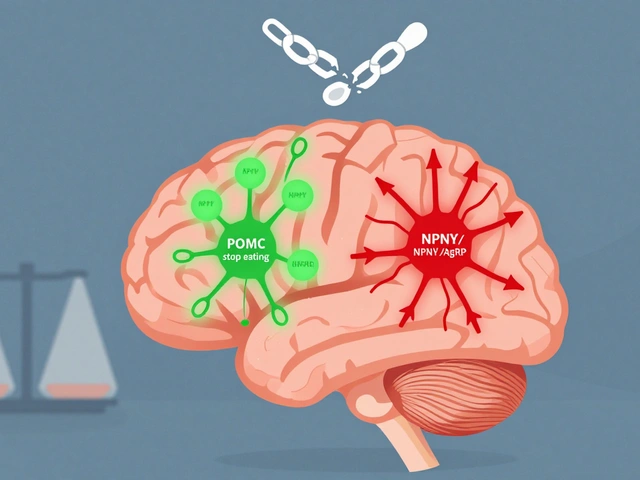
Most of the risk genes converge on two core pathways: dopamine signaling and iron metabolism. Both are essential for proper motor control and sensory perception.
- Dopamine a neurotransmitter that regulates movement and reward - Variants in BTBD9 and MEIS1 can alter dopamine receptor density or release, leading to the “restless” sensation.
- Iron deficiency low brain iron stores impair dopamine synthesis - Genes like PNPLA3 affect hepatic iron handling, indirectly influencing brain iron levels.
Animal models that knock out MEIS1 develop iron‑deficient “RLS‑like” behaviors, supporting a causal link. Meanwhile, NOS1 variants may disrupt nitric oxide signaling, which indirectly modulates dopamine release.
Should You Get Genetic Testing?
Genetic testing for RLS isn’t routine, but it becomes valuable in specific scenarios:
- Strong family history: If multiple first‑degree relatives have moderate or severe RLS, a panel that includes MEIS1, BTBD9, and NOS1 can clarify risk.
- Early‑onset disease: Onset before age 30 often signals a stronger genetic component.
- Research participation: Joining a GWAS cohort can give you access to testing at no cost while contributing to science.
Typical panels use saliva kits and report results in a few weeks. Results are expressed as “presence of risk allele” rather than a deterministic diagnosis. Importantly, a positive result only raises probability; environmental factors still determine whether symptoms manifest.
Implications for Family Members
If you carry a risk allele, your children inherit a 50% chance of receiving the same variant. However, penetrance-the chance that a carrier actually develops RLS-is modest (around 20‑30% for the most common alleles). Counseling focuses on:
- Monitoring early signs in relatives.
- Optimizing iron status through diet or supplementation, especially during pregnancy.
- Educating about lifestyle triggers: caffeine, nicotine, and certain antidepressants.
Family‑based studies suggest that proactive iron monitoring can lower symptom severity even among genetically predisposed individuals.

Managing RLS with a Genetic Lens
Knowing your genetic risk can guide treatment choices. For example, people with BTBD9 variants often respond well to low‑dose dopamine agonists (pramipexole or ropinirole) but may develop augmentation-worsening symptoms over time-more quickly. In such cases, clinicians may prioritize non‑dopaminergic options such as gabapentin enacarbil or iron supplementation.
Practical steps:
- Check ferritin levels: Aim for serum ferritin >75µg/L before initiating medication.
- Trial a short‑acting dopamine agonist: Start low, assess after 4 weeks.
- Review genetic report: If BTBD9 is present, schedule follow‑up at 3‑month intervals to watch for augmentation.
- Lifestyle tweaks: Stretching, leg massages, and a regular sleep schedule reduce symptom frequency.
These strategies align with the 2023 International RLS Guideline, which now recommends genetic information as an adjunct to clinical decision‑making.
Future Directions: What’s on the Horizon?
Research is moving toward polygenic risk scores (PRS) that combine many small‑effect variants into a single risk number. Early trials suggest PRS can predict which patients will benefit most from iron therapy versus dopamine agents. By 2025, several commercial labs plan to offer RLS‑specific PRS as part of broader sleep‑disorder panels.
Another exciting area is CRISPR‑based functional studies that edit MEIS1 in neuronal cultures, revealing precise mechanisms that could become drug targets. While therapy based on gene editing remains years away, the knowledge gained is sharpening our understanding of why some people develop RLS while others don’t.
Frequently Asked Questions
Can I inherit Restless Leg Syndrome?
Yes. Family studies show a heritability of about 50%. Specific gene variants such as MEIS1, BTBD9, and NOS1 raise the odds, but they don’t guarantee you’ll develop symptoms.
Is genetic testing covered by insurance?
Coverage varies. Some insurers reimburse panels ordered by a neurologist when there is a strong family history. It’s best to check your policy or ask the testing lab about pre‑authorization.
Do risk genes affect treatment response?
Research suggests BTBD9 carriers may experience faster augmentation with dopamine agonists, while MEIS1 carriers often improve with iron supplementation. Discuss your genetic results with your doctor to tailor therapy.
Should my children be tested?
Testing children is generally not recommended unless they already show symptoms. Monitoring iron status and early symptom awareness is a safer first step.
How reliable are current genetic findings?
The five risk genes listed have been replicated in multiple European cohorts and in meta‑analyses up to 2024. However, they explain only 10‑15% of the total genetic risk, so results should be interpreted as part of a broader clinical picture.





Reading this piece reminded me how often we ignore the human toll behind cold statistics. The author glosses over the suffering families endure, treating RLS like a lab result rather than a night‑time nightmare. While the genetics are fascinating, the emotional weight deserves more than a bland data dump. I wish the article had acknowledged the frustration patients feel when treatment fails.
Absolutely, the article does a solid job breaking down complex genetics into digestible steps. It’s encouraging to see practical tips alongside the science.
Great overview! The way you tied MEIS1 and iron metabolism makes the mechanistic picture clearer. I also appreciate the clear table summarizing risk alleles-those numbers are handy for clinicians. One thing to keep in mind is that allele frequencies differ across ethnic groups, so the European focus might miss important variations elsewhere. For patients, emphasizing iron supplementation before jumping to dopamine agonists is a prudent approach. Overall, this is a valuable resource for both doctors and patients.
The exposition, while comprehensive, suffers from occasional redundancies that dilute its scholarly impact. A more disciplined structure would benefit readers accustomed to the rigour of peer‑reviewed literature. Moreover, the omission of recent African cohort data constitutes a notable gap in the presented epidemiology. I recommend integrating these findings to enhance the article’s global relevance.
Thanks for laying out the genetics in a way that doesn’t feel overwhelmng. I’ve been dealing with my dad’s RLS for years, and the iron‑status advice hit home. It’s comforting to know there’s solid science behind the supplements we’ve been using. The section on family monitoring is especially useful for our whole household. Keep up the good work!
Your heartfelt anecdote, while commendable, hardly substitutes for rigorous genotype‑phenotype correlation. One must appreciate the elegance of polygenic risk scores, a marvel far beyond anecdotal iron tablets. The discourse would benefit from invoking the lexicon of systems biology rather than mere bedside narratives. In sum, a more erudite tone would elevate the discussion to its deserved academic stature.
Listen, if you think taking a random iron pill will solve everything, you’re mistaken. Real genetic risk needs proper testing, not just guesswork. Stop flippin' around and get a proper panel!
Your point about untested supplementation is well‑taken; however, the pharmacogenomic implications merit deeper exploration. Conducting a genotype‑guided therapeutic algorithm could mitigate augmentation risk associated with dopaminergic agents. Integrating biomarkers such as serum ferritin into the decision matrix aligns with precision‑medicine standards. Thus, a systematic approach supersedes ad‑hoc supplementation.
Genetics give us a roadmap, but lifestyle is the engine.
Sure, they love to hand you a genetic panel while the pharma giants sit back and watch the profit racks climb. Behind the glossy brochure lies a hidden agenda to push expensive meds over simple iron fixes. Stay wary of the marketing spin.
The data presented, albeit extensive, lack a critical appraisal of methodological limitations.
I hear you, but the study design wasnt robust enough to draw firm conclusions. We need larger, diverse cohorts to validate these SNP associations. Until then, keep the hype in check.
Oh great, another article telling us to check ferritin – because we all have time to order labs on a Sunday! ‽ Seriously, why not just add a line that says “buy the supplement and hope for the best”? ‽ The authors clearly think genetics will solve all our bedtime woes. ‽ Yet they forget most patients can’t even afford a basic Iron tablet. ‽
The intersection of neurogenetics and sleep physiology offers a fertile ground for philosophical inquiry. One might argue that the very concept of a ‘risk allele’ is a reductionist abstraction that masks the lived experience of restless nights. Yet, the empirical mapping of MEIS1, BTBD9, and their downstream pathways provides a concrete scaffold upon which to build therapeutic strategies. From a systems‑level perspective, the dopaminergic circuitry functions as a finely tuned orchestra, where a single discordant note can reverberate as motor restlessness. Iron homeostasis, meanwhile, acts as a silent conductor, subtly modulating neurotransmitter synthesis. When genetic predisposition aligns with iron deficiency, the resultant symphony is one of maladaptive excitation. Clinical practice thus faces a dual imperative: to correct the biochemical deficiency and to respect the genomic backdrop. Polygenic risk scores, though still nascent, promise to quantify the cumulative burden of numerous minor variants. Critics warn that such scores risk becoming deterministic, stripping patients of agency. Conversely, proponents view them as navigational tools, guiding clinicians toward personalized interventions. The ethical dimension cannot be ignored; disclosing a modest risk may generate anxiety without actionable benefit. Moreover, the socioeconomic disparities in access to genetic testing exacerbate existing health inequities. Future research should therefore prioritize inclusive cohorts that reflect global diversity. Only then can we claim that the genomic narrative is truly universal rather than Eurocentric. In the meantime, clinicians must balance cutting‑edge genetics with timeless basics like sleep hygiene and iron supplementation. Thus, the story of restless leg syndrome is not merely a tale of genes, but a broader meditation on how biology, environment, and human agency intertwine.
Great synthesis of the science and its larger meaning. Your balanced view will help many clinicians see beyond the numbers.
While the article is thorough, it neglects the socioeconomic context of genetic testing. A broader lens would improve its relevance.
Totally get where you're coming from – it's easy to miss the bigger picture when diving into data. A little perspective goes a long way.
Reading this stuff can be overwhelming, especially when you’re dealing with a loveds’ sleepless nights. I felt a wave of relief when the piece stressed iron checks before meds. Keep looking out for those simple steps, they really matter.
Your encouragement is exactly what folks need right now – a little hope goes a long way. Stay positive and keep pushing for better sleep!