What Happens to Your Body After a Medication Overdose?
Most people think of a medication overdose as a one-time emergency - something you survive, then move on from. But if you’ve lived through it, or know someone who has, you know it’s not that simple. Even if you wake up in the hospital, breathe on your own, and walk out with a clean bill of health, your body may still be paying the price months or years later. The truth is, medication overdose doesn’t end when the antidote is given or the breathing machine is turned off. For many, it’s just the beginning of a long, hidden recovery.
Brain Damage Isn’t Always Obvious
The most damaging effect of an overdose isn’t always visible. It doesn’t show up on an X-ray or blood test right away. It hides in your brain. When you overdose on opioids, benzodiazepines, or even too much acetaminophen, your breathing slows or stops. That means your brain isn’t getting enough oxygen. After just four minutes without oxygen, brain cells start dying. That’s faster than it takes to call 911 in many places.
Survivors often describe it as ‘brain fog’ - a constant feeling of being slow, spaced out, or unable to think clearly. One man from South Carolina told his doctor, ‘I used to be able to fix cars by ear. Now I can’t remember how to turn the ignition key.’ Studies show 63% of overdose survivors have trouble with memory. Nearly 57% struggle to focus. And 38% lose fine motor control - meaning they drop things, trip, or can’t button a shirt without help.
It’s not just memory. Overdose survivors report trouble speaking, hearing, making decisions, and even recognizing faces. These aren’t temporary side effects. They’re permanent changes. A 2023 study found that people who went without oxygen for more than 10 minutes were over three times more likely to have lasting brain damage than those who got help within five minutes.
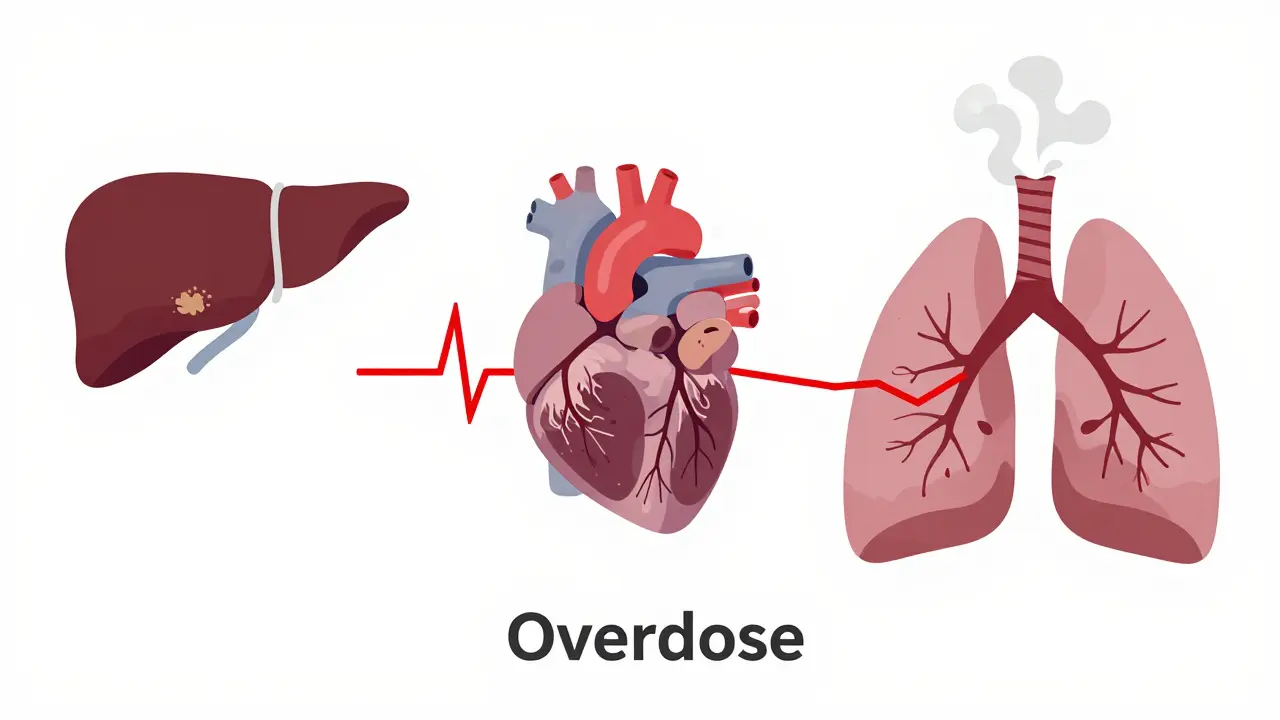
How Different Drugs Hurt Different Organs
Not all overdoses are the same. The drug you took determines what parts of your body get damaged - and how badly.
Opioids like oxycodone, fentanyl, or tramadol cause breathing to stop. That leads to low oxygen, which can trigger kidney failure in 22% of cases, heart rhythm problems in 18%, and strokes in 8%. Many also develop pneumonia from inhaling vomit during the overdose. These aren’t just ‘complications.’ They become lifelong conditions.
Benzodiazepines - drugs like Xanax or Valium - don’t usually stop breathing as quickly, but they depress the brain for hours. Survivors often say they feel like they’re walking through fog even after six months. One in four have trouble remembering things or making simple choices. Their brains don’t recover the same way they used to.
Stimulants like Adderall or Ritalin, when taken in large doses, overload the heart. Over time, 31% of survivors develop high blood pressure or irregular heartbeats. Some even suffer heart attacks years later. And because these drugs flood the brain with dopamine, 19% end up with lasting anxiety, paranoia, or hallucinations.
And then there’s acetaminophen - the common painkiller in Tylenol. It doesn’t make you pass out. You feel fine for days. But if you take too much, your liver starts dying. By the time you feel sick, it’s often too late. Nearly half of those who wait more than eight hours to get treatment end up with cirrhosis or liver failure. That’s not a guess. That’s what the Journal of Hepatology found in 2022.
The Mental Health Toll Nobody Talks About
Surviving an overdose doesn’t mean you’re ‘better.’ It just means you’re alive. But many survivors carry a heavier burden: trauma.
More than 70% develop a new mental health condition after an overdose. For 41%, it’s PTSD. They relive the moment they couldn’t breathe. For 38%, it’s major depression. For 33%, it’s constant, crushing anxiety. And here’s the cruel part - most of them don’t get help. Only 28% see a mental health professional within 30 days of leaving the hospital.
One woman in Atlanta told her therapist, ‘I survived, but I don’t know who I am anymore. I used to be a teacher. Now I can’t even remember my students’ names.’ That’s not just grief. That’s brain injury combined with psychological trauma. And it’s not rare. The Substance Abuse and Mental Health Services Administration found that overdose survivors are nearly five times more likely to develop depression than people who use drugs but never overdose.
Why Most People Don’t Get the Care They Need
Here’s the hard truth: hospitals treat overdoses like emergencies - not chronic conditions. They stabilize you. They give you naloxone. They check your vitals. And then they send you home with a pamphlet.
But what about the brain damage? The liver scarring? The memory loss? The panic attacks that start at 3 a.m.?
Only 47% of emergency rooms document what follow-up care a survivor might need. And 41% are discharged without any referral to a specialist. That’s not negligence. It’s the system. There aren’t enough neurologists, addiction counselors, or liver specialists trained to handle long-term overdose aftercare.
Even when care is available, it’s often out of reach. In rural areas, it can take over 20 minutes to get naloxone to someone who’s overdosing. In cities, it’s hard to find a therapist who understands the difference between addiction and brain injury. And insurance? Most plans won’t cover cognitive rehab for ‘drug-related’ damage. They call it ‘pre-existing.’

What Recovery Really Looks Like
Recovery isn’t about quitting drugs. It’s about rebuilding a broken body and mind.
Some survivors work with speech therapists to regain lost language skills. Others do physical therapy to fix balance problems. A few get cognitive training to help their brains relearn how to remember things. But none of this is easy. And none of it is guaranteed.
One man in Florida spent two years in rehab after an oxycodone overdose. He still can’t drive. He forgets birthdays. He gets lost in his own neighborhood. But he’s alive. And he’s trying. He says, ‘I don’t expect to be who I was. I just want to be someone who can hold my grandkid without shaking.’
There’s no magic cure. But early intervention helps. If you or someone you know overdosed, get a brain scan. Get a liver test. See a neurologist. Talk to a therapist. Don’t wait for symptoms to get worse. They won’t fix themselves.
What’s Being Done - and What’s Not
There’s hope. In 2023, the U.S. government gave $156 million to study how overdoses accelerate brain aging. That’s the first time this has ever happened. Doctors now know that each overdose can make your brain age 7 years faster than normal.
The American Medical Association now requires hospitals to check survivors for brain injury within 72 hours. That’s progress. But only 19% of U.S. hospitals have formal protocols for this. And in rural counties, only 31% have access to any kind of neurological rehab.
The cost of ignoring this? The average lifetime care for someone with permanent brain damage from an overdose is over $1.2 million. That’s not just a number. That’s a family’s savings, a job lost, a child’s future put on hold.
Final Thoughts: This Isn’t Just About Drugs
Medication overdose isn’t a moral failure. It’s a medical crisis with long-term consequences that no one talks about. We focus on stopping deaths. But what about the thousands who survive - and live with broken brains, failing organs, and invisible trauma every day?
If you’ve ever overdosed, or know someone who has, you deserve more than a second chance. You deserve a full recovery plan. Your brain matters. Your body matters. And the damage isn’t your fault.
Ask for help. Push for care. Don’t let anyone tell you you’re ‘lucky to be alive’ and leave it at that. You’re alive - now make sure you’re really living.





So now we're treating overdose survivors like fragile porcelain dolls? Wake up. If you're dumb enough to OD, you gotta live with the consequences. Nobody owes you a second chance, let alone a neurologist and a therapist. Stop whining and take responsibility.
This is one of the most important pieces I've read all year. The way you lay out the hidden toll-brain fog, memory loss, organ damage-isn't just medical, it's human. I've watched someone I love go through this, and no one talks about how the silence after survival is the loudest part. Thank you for naming what so many suffer through alone.