Most people assume their prescriptions come in standard pills or capsules from big drugmakers. But for thousands of patients, that’s not enough. Sometimes, the only way to get the right dose, avoid an allergy, or make a medication swallowable is through a compounded medication. These aren’t mass-produced drugs. They’re made by hand, one at a time, in a pharmacy, to fit a single person’s needs.
Why Standard Pills Don’t Work for Everyone
Commercial drugs are made for the average patient. But what if you’re not average? What if you’re allergic to the dye in your blood pressure pill? Or your child can’t swallow a tablet? Or you need a dose that doesn’t exist - like 1.5 mg of a drug that only comes in 1 mg or 2 mg? That’s where compounding steps in. Up to 5% of patients need something that factory-made drugs can’t provide. For kids, flavored liquid versions of ADHD meds can boost adherence from 40% to 95%. For older adults with trouble digesting pills, a topical cream can deliver medication through the skin instead. For people with lactose intolerance or gluten sensitivity, a compounded version removes those triggers entirely. One study found that 15 million Americans react to common ingredients like dyes or preservatives in commercial drugs. Compounding removes those risks.What Compounded Medications Can Do
A compounding pharmacist doesn’t just mix pills. They rebuild medications from scratch. They can:- Change the dosage to match exact needs - not just 5 mg or 10 mg, but 7.3 mg if that’s what’s right for you
- Turn a pill into a liquid, gel, cream, suppository, or even a lollipop
- Remove allergens like gluten, dairy, soy, or artificial colors
- Combine five different pills into one easy-to-take dose
- Create hormone therapies with exact ratios of bioidentical hormones
- Formulate pain creams that target joint pain without flooding the body with opioids
The Hidden Risks
But here’s the catch: compounded medications aren’t FDA-approved. That means no one tested them for safety or effectiveness before you took them. The FDA doesn’t check batches. They don’t guarantee purity. And when things go wrong, the consequences can be deadly. The 2012 fungal meningitis outbreak tied to contaminated steroid injections from a compounding pharmacy killed 64 people and sickened nearly 800. That disaster changed everything. Since then, the FDA has cracked down on large-scale compounding operations that act like drug manufacturers. But small, local pharmacies still operate under looser rules. Between 2010 and 2020, compounded drugs made up just 1% of prescriptions but caused 17% of drug recalls. Why? Because quality control varies wildly. One pharmacy might use sterile techniques and test every batch. Another might skip basic steps to save time. A patient on Reddit shared how their compounded thyroid med had inconsistent strength - causing wild swings in their TSH levels. That’s not rare. One survey found 18% of patients using compounded meds had to get them redone due to quality issues.
Who Should Use Them - and Who Shouldn’t
Compounded medications aren’t for everyone. They’re not cheaper alternatives to FDA-approved drugs. They’re not for people who just want a different flavor or a “natural” version of a medication that already exists. They’re for people with real, documented needs:- Patients allergic to inactive ingredients in commercial drugs
- Children or elderly who can’t swallow pills
- People needing doses not available on the market
- Those requiring combination therapies that don’t exist as a single pill
- Patients with rare conditions where no commercial option exists
How to Find a Safe Compounding Pharmacy
Not all compounding pharmacies are equal. Out of 7,500 pharmacies in the U.S. that offer compounding, only about 350 are accredited by the Pharmacy Compounding Accreditation Board (PCAB). That’s less than 5%. Look for that badge. Ask your pharmacist:- Are you PCAB-accredited?
- Do you follow USP Chapter <795> for non-sterile compounds or <797> for sterile ones?
- How do you test your batches for potency and purity?
- Do you use a cleanroom for sterile preparations?

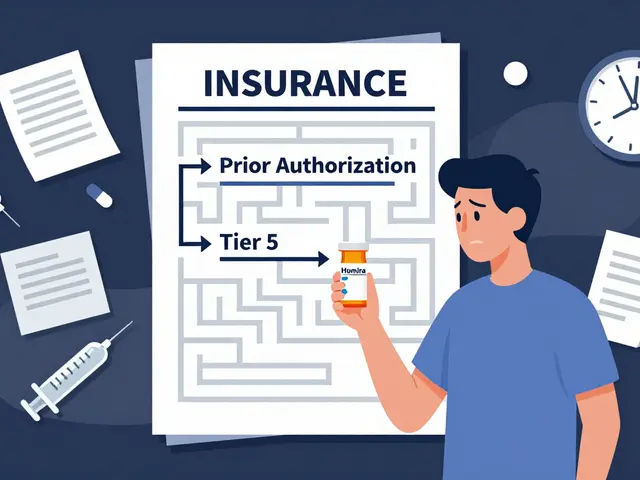
Cost and Insurance: What to Expect
Compounded meds cost more. A simple non-sterile compound might run $30-$100. A sterile injection or IV solution could hit $200-$500. Compare that to a $10 generic pill. The price difference comes from labor, specialized equipment, testing, and small-batch production. Insurance coverage is spotty. Medicare Part D covers only 42% of compounded claims. Private insurers vary. Some require prior authorization. Others won’t touch them at all. Always check with your insurer before filling the prescription. You might need to pay out-of-pocket - and that’s okay if the alternative is no treatment at all.The Future of Personalized Medicine
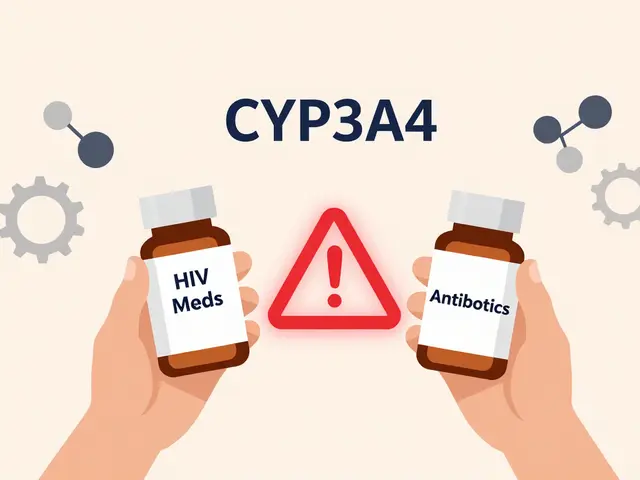
The future of compounding is getting smarter. Some pharmacies are now using genetic testing to tailor medications. For example, if you have a CYP2D6 gene variant that affects how your body processes certain drugs, your pharmacist can adjust the dose or formula to match your biology. Early results show 30% better outcomes in patients using this approach. But regulation is catching up. The 2022 Compounding Quality Act requires outsourcing facilities to report side effects and follow strict quality systems. The FDA is also cracking down on pharmacies compounding drugs like semaglutide in large volumes - treating them like manufacturers, not pharmacies. The goal isn’t to eliminate compounding. It’s to protect patients while preserving access for those who truly need it.When to Talk to Your Doctor About Compounding
If you’re struggling with side effects, swallowing pills, or your meds just don’t seem to work right - don’t assume it’s your fault. Ask your doctor: “Is there a compounded version of this medication that might work better for me?” Bring up:- Allergies to dyes, preservatives, or fillers
- Difficulty swallowing tablets or capsules
- Need for a specific dose that isn’t available
- Side effects from commercial versions
- Need for a different form - like a cream instead of a pill
Are compounded medications safe?
They can be, but only if made by a qualified, accredited pharmacy under strict standards. Unlike FDA-approved drugs, compounded medications aren’t tested for safety or effectiveness before use. The risk comes from poor quality control, not the concept itself. Always choose a PCAB-accredited pharmacy and ask about their testing protocols.
Can I get compounded medications without a prescription?
No. Federal law requires a valid prescription from a licensed provider for any compounded medication. Pharmacies that sell them without one are breaking the law. Be wary of online sellers offering “hormone creams” or “weight loss formulas” without a prescription - these are often unsafe and illegal.
How do I know if my compounding pharmacy is reputable?
Look for PCAB accreditation - only about 350 out of 7,500 compounding pharmacies in the U.S. have it. Ask if they follow USP <795> or <797> standards. Check if they use a cleanroom for sterile products and test each batch for potency and purity. Avoid pharmacies that sell bulk quantities or advertise products online without requiring a prescription.
Why are compounded medications so expensive?
They’re made by hand, one patient at a time, using specialized equipment and high-quality ingredients. Unlike factory-made drugs, there’s no mass production to lower costs. Sterile compounds require cleanrooms, testing, and trained staff - all adding to the price. A simple cream might cost $50, while a sterile injection could be $400.
Will my insurance cover compounded medications?
Maybe. Medicare Part D covers only 42% of compounded claims. Private insurers vary widely. Some require prior authorization, others won’t cover them at all. Always check with your plan before filling the prescription. You may need to pay out-of-pocket, especially for complex formulations.




Compounding is just pharmacy magic when the big pharma bots fail. I got my kid a cherry-flavored Adderall that doesn't taste like regret. 95% adherence? More like 100% because she actually takes it. No more screaming at breakfast.
I had a bad reaction to a compounded thyroid med. One batch was fine, next one spiked my TSH. No one tested it. Just trust the guy in the lab coat.
Look, I'm from Texas and I've seen my grandma take a cream for her arthritis that worked better than the pills. But I also know a guy whose wife got sick from a bad batch of compounded estrogen. It's not about if it works-it's about who's making it. PCAB accreditation isn't optional. It's your lifeline.
My cousin with Lyme disease got a custom IV combo that finally brought her pain down. She was on 12 pills a day before. Now it's one slow drip. No more nausea. No more pills she couldn't swallow. This isn't fringe medicine-it's survival. And yeah, it cost $350. Worth every penny when you're not vomiting all day.
Big Pharma hates this. They don't want you to know you can bypass their overpriced, dye-filled pills. The FDA cracked down because compounding pharmacies were making too much money. They don't want competition. That's why they make it sound scary. You think the 2012 outbreak was the only one? Nah. They buried the rest.
Let’s be real. Compounding is just pharma’s loophole for charging $400 for a jar of cream that’s 80% glycerin. If you need a 7.3 mg dose, you’re either a medical anomaly or you’re being scammed by a guy in a basement with a blender. I’ve seen the receipts.
i got a compoound pain cream and it was like magic. no more opioids. no more stomach issues. but then the next batch was weak as hell. i think they used tap water. who knows. i just got it from a place that said "we make it fresh daily" on their sign. lol. maybe i got lucky.
Has anyone tracked long-term outcomes for compounded hormone therapies? I’m curious if the variability in potency affects things like bone density or cardiovascular risk over time.
The FDA doesn't approve compounded drugs because they're not mass-produced-not because they're inherently dangerous. The real issue is inconsistent regulation across states. Until there's federal oversight on quality standards, patients are gambling with their health.
It's important to recognize that compounding isn't a panacea, nor is it a rebellion against pharmaceutical industry norms. It is, fundamentally, an extension of clinical pharmacology into the realm of individualized care. When a patient has documented allergies, physiological limitations, or unique metabolic profiles, the ability to tailor medication becomes not just a convenience, but a medical necessity. The ethical obligation lies not in rejecting compounding, but in ensuring that those who provide it are held to the highest standards of training, sanitation, and accountability. We must not confuse the occasional failure of unregulated operations with the broader, life-sustaining utility of the practice.
I know someone who lost her mom because of a compounded med. They said it was "sterile" but the lab had mold in the vents. Now I won’t even let my dog near a compounded prescription. It’s a lottery with your life.
To those dismissing compounding as risky: consider this. For children with severe food allergies, a compounded version of their seizure medication without corn starch or dairy is the only way they can take it at all. For elderly patients with dysphagia, a topical gel is the difference between hospitalization and independence. The risks are real-but so are the consequences of denying access. The solution isn’t to ban compounding. It’s to fund accreditation, mandate batch testing, and require transparency. We owe that to the patients who have no other options.