Imagine waking up after eight hours of sleep, but still feeling like you haven’t slept at all. You sit down to work, and within minutes, your eyes close - no matter how hard you try to stay awake. This isn’t laziness. It’s not just being tired. This is narcolepsy, a neurological disorder that hijacks your brain’s ability to control sleep and wakefulness. People with narcolepsy don’t just feel sleepy - they experience sudden, uncontrollable sleep attacks, sometimes mid-sentence, mid-step, even while driving. It’s not rare. About 1 in every 2,000 people has it. And for most, the first sign isn’t nightmares or muscle weakness - it’s overwhelming daytime sleepiness that no amount of coffee can fix.
What Narcolepsy Really Feels Like
Narcolepsy isn’t just about falling asleep at random times. It’s a five-part symptom package that can turn daily life into a minefield. The most universal symptom - present in every single case - is excessive daytime sleepiness (EDS). Patients report 4 to 6 sleep attacks per day, each lasting 15 to 30 minutes. Afterward, they wake up feeling refreshed… for about 20 minutes. Then it starts again. No matter how much they sleep at night, the brain keeps hitting a reset button.
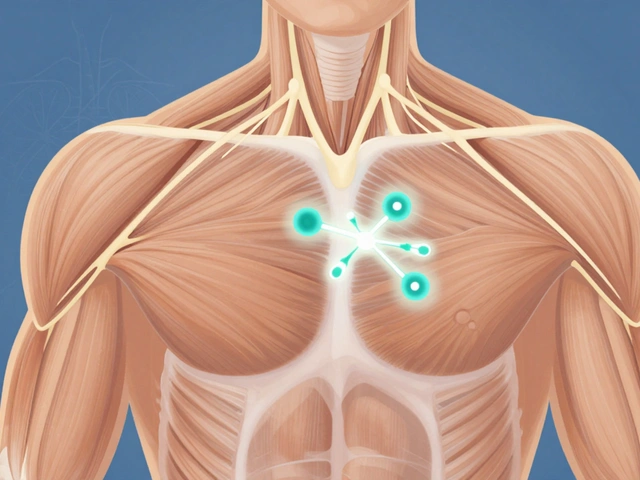
For about 70% of people, there’s another terrifying symptom: cataplexy. One moment you’re laughing at a joke, the next, your knees buckle. Your head drops. Your jaw goes slack. You’re fully awake - you can hear, see, think - but your body won’t respond. These episodes last seconds to minutes, triggered by strong emotions like joy, anger, or surprise. It’s not fainting. It’s not a seizure. It’s a sudden, temporary shutdown of muscle control, caused by the brain’s failure to regulate the boundary between wakefulness and REM sleep.
Then there’s sleep paralysis. You wake up - or fall asleep - and can’t move. You’re conscious, terrified, but your muscles are locked. Sometimes, hallucinations come with it: ghostly figures in the room, voices whispering, pressure on your chest. These aren’t dreams. They’re hallucinations happening while you’re wide awake. About 75% of people with narcolepsy get them. And nighttime sleep? It’s broken. You might spend 8 hours in bed, but you’re waking up 4 to 6 times. You never get deep, restorative sleep.
Diagnosis: It’s Not Just Tiredness
Many people live for years thinking they’re just lazy, depressed, or stressed. Doctors often misdiagnose narcolepsy as depression, epilepsy, or even ADHD. The real diagnosis requires two key tests. First, an overnight sleep study (polysomnography) to rule out sleep apnea or other disorders. Then, the Multiple Sleep Latency Test (MSLT) - a series of 5 naps spaced two hours apart. If you fall asleep in under 8 minutes on average, and enter REM sleep in at least two of those naps, that’s a diagnostic red flag.
There’s also a blood test and spinal fluid test. If your cerebrospinal fluid shows hypocretin-1 levels below 110 pg/mL, you have Type 1 narcolepsy. That’s the version linked to cataplexy and an autoimmune attack on the brain cells that produce hypocretin - a chemical that keeps you awake. Without it, your brain can’t maintain wakefulness. Type 2 narcolepsy has the same sleepiness but no cataplexy and normal hypocretin levels. It’s harder to diagnose, but just as disabling.
Stimulants: The First-Line Treatment
There’s no cure. But there are treatments that work. For excessive daytime sleepiness, stimulants are the first line of defense. Not the kind you think of - not caffeine or energy drinks. These are prescription medications that target the brain’s wakefulness systems.
Modafinil (Provigil) and armodafinil (Nuvigil) are the most commonly prescribed. They don’t work like amphetamines. Instead, they gently boost dopamine and help stabilize the orexin system - the same system that’s damaged in narcolepsy. In clinical trials, about 70% of patients saw their sleepiness scores drop by 5 points or more on the Epworth Sleepiness Scale. That’s the difference between falling asleep at your desk and staying alert through a meeting.
Armodafinil lasts longer - about 15 hours - so one pill in the morning can cover your whole day. Modafinil is cheaper, especially now that it’s generic. Many patients say it gives them “clean energy” - no jitteriness, no crash. But it doesn’t work forever. About 40% report diminishing effects after 18 months. Headaches and nausea are common side effects, but serious ones are rare.

Traditional Stimulants: More Power, More Risk
When modafinil doesn’t cut it, doctors turn to stronger options: methylphenidate (Ritalin) or amphetamines (Adderall). These are powerful. Up to 80% of patients respond. They can turn someone who couldn’t hold a job into someone who can work full-time. Sarah Johnson, a 34-year-old teacher, went from an Epworth score of 18 (severe sleepiness) to 6 on armodafinil - and got her career back.
But the cost is high. These drugs raise blood pressure and heart rate. They cause appetite loss, anxiety, and emotional blunting. One in two people on long-term amphetamines stops taking them because of side effects. And there’s a risk of abuse. That’s why they’re Schedule II controlled substances - the same category as cocaine and oxycodone. Doctors require regular ECGs and blood pressure checks. They’re not for everyone. But for severe cases, they’re life-changing.
Newer Options and What’s Coming
There are newer drugs that offer alternatives. Pitolisant (Wakix) works by boosting histamine in the brain - a natural wakefulness signal. It’s as effective as modafinil but doesn’t raise blood pressure. The catch? It costs $850 a month - more than double generic modafinil. Solriamfetol (Sunosi) blocks dopamine and norepinephrine reuptake. It gives strong wakefulness with low abuse risk, but 7% of users develop high blood pressure.
And then there’s sodium oxybate (Xyrem). It’s not a stimulant. It’s a sedative taken at night. But it improves both cataplexy and daytime sleepiness. Eighty-five percent of patients see fewer cataplexy attacks. But it’s tightly controlled - you can only get it through a special pharmacy, and you must take it twice a night. The sodium content can be dangerous for people with heart problems.
On the horizon: drugs that actually fix the root problem. TAK-994, an orexin receptor agonist, showed huge promise in trials - reducing sleepiness by nearly 8 points. But development was paused due to liver concerns. Researchers are now working on therapies that could stop the autoimmune attack on hypocretin cells, or even replace them. That’s the future. But for now, we still rely on stimulants to keep people awake.

Living With Narcolepsy
Medication alone isn’t enough. The best outcomes come from combining drugs with lifestyle changes. Scheduled naps - even 15 minutes - can reduce sleep attacks. Avoiding alcohol and heavy meals helps. Workplaces are starting to adapt. Under the Americans with Disabilities Act, employers must offer accommodations: flexible hours, quiet spaces for naps, adjusted deadlines.
But getting treatment is hard. Insurance often denies coverage. The average wait for prior authorization is 14 days. Many patients stay on low doses because they can’t afford to escalate. Others give up after years of misdiagnosis. The Narcolepsy Network estimates 100,000 people in the U.S. alone are still undiagnosed.
There’s no shame in needing help. Narcolepsy isn’t a choice. It’s a brain disorder. And stimulants - whether modafinil, armodafinil, or something stronger - aren’t crutches. They’re tools. Tools that let people work, drive, parent, live. Without them, many would be trapped. With them, they can breathe.
Can narcolepsy be cured?
No, there is no cure for narcolepsy yet. Current treatments manage symptoms - especially daytime sleepiness and cataplexy - but they don’t fix the underlying loss of hypocretin-producing brain cells. Research is ongoing into disease-modifying therapies, including immunotherapy and cell replacement, but these are still in early stages.
Is modafinil addictive?
Modafinil has a very low potential for addiction compared to traditional stimulants like Adderall. It doesn’t cause the dopamine spike associated with abuse. The FDA doesn’t classify it as a controlled substance. However, some users report tolerance over time, meaning they need higher doses for the same effect - which is different from addiction.
Why do some people with narcolepsy gain weight?
Narcolepsy itself can slow metabolism and disrupt appetite hormones. Many patients report increased hunger, especially for carbs. While stimulants like modafinil may suppress appetite, others like sodium oxybate can cause weight gain. Lack of physical activity due to fatigue also contributes. Weight management often requires dietary planning and structured exercise.
Can you drive with narcolepsy?
Many people with narcolepsy drive safely - but only if their symptoms are well-controlled with medication and naps. Some states require doctors to report diagnosed patients to the DMV. If you have frequent sleep attacks or uncontrolled cataplexy, driving is unsafe. Always follow your doctor’s advice and never drive if you feel drowsy.
What happens if you stop taking stimulants suddenly?
Stopping stimulants abruptly can cause rebound sleepiness, fatigue, irritability, and depression. For some, it feels like falling into a deep, unbreakable sleep. Never stop these medications without medical supervision. Tapering down slowly under a doctor’s guidance helps avoid withdrawal symptoms and keeps sleepiness manageable.
Next Steps if You Suspect Narcolepsy
If you’ve been feeling exhausted despite sleeping enough - and you’re having sudden muscle weakness, hallucinations, or sleep paralysis - talk to a sleep specialist. Don’t wait. Start with your primary doctor and ask for a referral to a sleep clinic. Bring a sleep diary: record when you sleep, when you feel sleepy, any emotional triggers, and whether you’ve had episodes of falling asleep unexpectedly.
Be ready for testing. The MSLT takes a full day. Insurance may delay approval. But if you’re diagnosed, you’re not alone. Support groups, like MyNarcolepsyTeam and the Narcolepsy Network, connect you with people who get it. And treatment works. You can get back to living - not just surviving.






Just had my first MSLT last week. Fell asleep in 3 minutes during the second nap. They told me I have Type 1. I’ve been told I’m lazy for 12 years. This article? It felt like someone finally described my life in words. Thank you.
Modafinil is overhyped. I’ve been on it for 5 years. It stops working. Then you get stuck with Adderall which turns you into a nervous wreck. The real problem? Doctors don’t care until you’re on the verge of losing your job. Then they act like heroes.
My daughter was diagnosed at 16. We went through three doctors who thought it was depression. The day she got her first prescription? She smiled for the first time in months. This isn’t about being lazy. It’s about brain chemistry. And yes, stimulants save lives.
Oh please. You’re all just addicted to stimulants and calling it ‘treatment.’ Wake up. You’re trading one dependency for another. If you just got more sleep, exercised, ate better-
Wait, you can’t. Because your brain won’t let you. Never mind.
The hypocretin deficiency model is elegant but incomplete. The autoimmune hypothesis suggests molecular mimicry post-infection-perhaps H1N1 or streptococcal triggers. But why only 1 in 2,000? Epigenetics likely modulates penetrance. The real frontier isn’t pharmacology-it’s neuroregeneration.
I’m not mad… I’m just disappointed. We have the science to fix this. We have the funding. But we don’t prioritize brain disorders unless they affect rich white men. My sister died waiting for insurance approval. This isn’t medicine. It’s a lottery.
As someone who’s been on armodafinil for 8 years, I can say this: it’s not perfect, but it’s the difference between existing and living. I coach youth soccer now. I didn’t think I’d ever be able to. Thank you for writing this with such clarity.
If you’re reading this and think you might have narcolepsy-don’t wait. Bring your sleep diary to your doctor. Ask for the MSLT. If they refuse, go to a sleep clinic. This isn’t something you grow out of. It’s something you manage. And you deserve to manage it well.
I’m from Canada and our healthcare system covered my sodium oxybate after two years of appeals. The twice-nightly dosing is brutal, but the reduction in cataplexy? Worth it. I’ve driven cross-country since starting it. That’s something I never thought I’d say. Also, avoid caffeine after 2 PM. It ruins everything.
And yes, I’ve had sleep paralysis while watching Netflix. It’s terrifying. But now I know it’s not ghosts. Just my brain being weird.
My brother has narcolepsy. He’s a firefighter. He takes his meds, naps before shifts, and never lets it stop him. People think he’s ‘crazy’ for needing a nap room at the station. But he’s saved three lives this year. You don’t need to be ‘normal’ to be heroic.
So let me get this straight-you’re proud of taking a drug that’s chemically similar to crystal meth, just because you’re ‘too tired’? What’s next? A pill for laziness? Maybe a pill for being bad at time management? Wake up, people. This isn’t a medical condition-it’s a failure of discipline.
I’m a Latina woman with narcolepsy. I had to fight my family to even get tested. ‘You’re just tired because you don’t pray enough.’ ‘Maybe you’re just depressed.’ I lost three jobs before I got diagnosed. Now I’m a nurse. I tell my patients: your brain isn’t broken. It’s just wired differently. And you’re not alone.
Just started modafinil last month. First day? I stayed awake through a 6-hour meeting without nodding off. I cried in the parking lot. I didn’t realize how much I’d been holding my eyes open with willpower alone. Thank you for this post. It helped me feel seen.
One thing no one talks about: the emotional toll. You learn to fake being awake. You smile through cataplexy. You lie about why you’re late. You stop telling people how you feel because they don’t believe you. The medication helps your body. But the healing? That takes time, therapy, and people who listen.
Life is illusion. Sleep is truth. We are all dreaming. Narcolepsy? Just a glimpse behind the veil.