What Is Polycystic Kidney Disease?
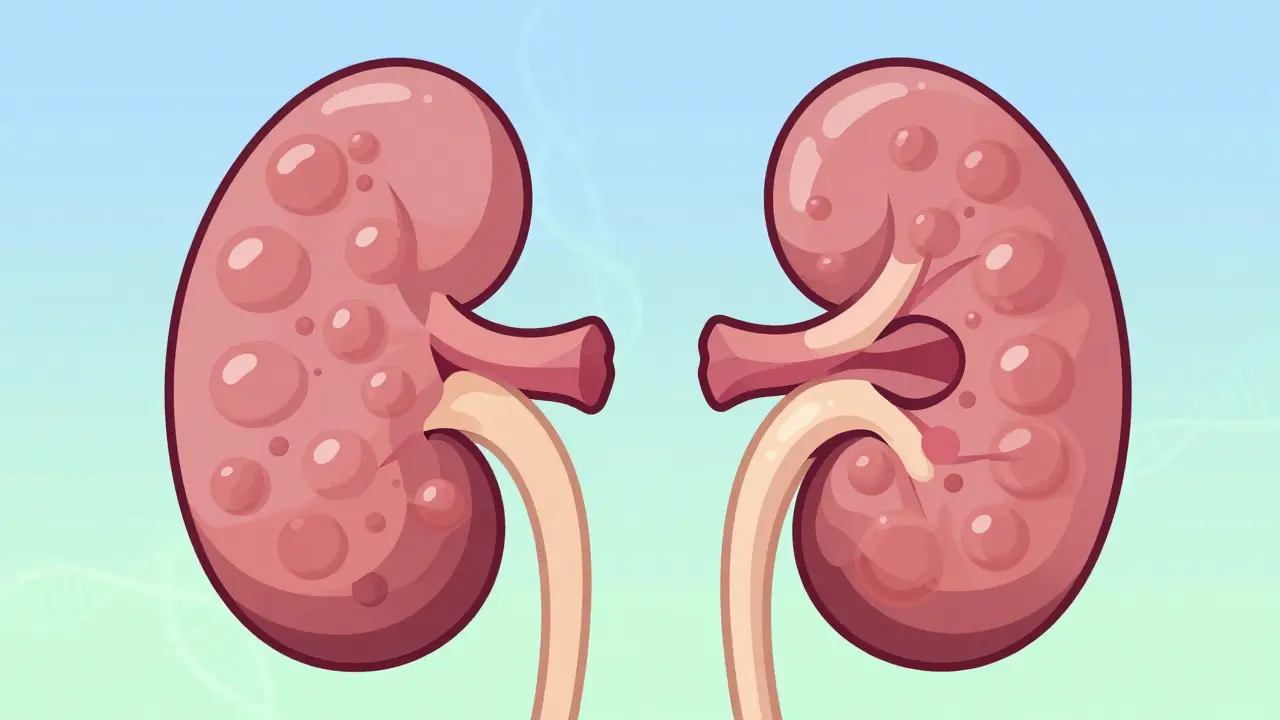
Polycystic kidney disease, or PKD, is a genetic condition where hundreds or even thousands of fluid-filled cysts grow inside the kidneys. These cysts don’t just sit there-they keep expanding, slowly crushing healthy kidney tissue until the organs can’t do their job anymore. By the time someone reaches their 60s or 70s, many with PKD end up needing dialysis or a kidney transplant. It’s not rare: about 1 in every 400 to 1,000 people have the most common form, called ADPKD. That means in a city like Durban, with over 1.5 million people, there could be more than 1,500 individuals living with this condition right now.
The Two Main Types: ADPKD and ARPKD
Not all PKD is the same. There are two major types, and they’re as different as day and night.
Autosomal Dominant Polycystic Kidney Disease (ADPKD) is by far the most common-making up over 98% of all cases. You only need to inherit one bad copy of either the PKD1 or PKD2 gene from one parent to get it. If your mom or dad has it, you have a 50% chance of getting it too. About 78% of ADPKD cases come from a mutation in PKD1, which tends to cause worse symptoms earlier. PKD2 is milder, with kidney failure often happening later in life.
Autosomal Recessive Polycystic Kidney Disease (ARPKD) is rare-only about 1 in 20,000 babies are born with it. To get ARPKD, you need two bad copies of the PKHD1 gene-one from each parent. If both parents are carriers (and don’t have the disease themselves), each child has a 25% chance of being affected. This type usually shows up right after birth or in early childhood. Babies with ARPKD often have enlarged kidneys and breathing problems from birth. Many don’t survive past infancy, but those who do face lifelong kidney and liver complications.
How Do You Know If You Have It?
Many people with ADPKD don’t feel sick until their 30s or 40s. But signs start building up long before symptoms appear. The most common early warning is high blood pressure. In fact, 89% of people with ADPKD develop hypertension by age 30. Other early signs include back or side pain, blood in the urine, frequent kidney infections, and unexplained swelling.
Doctors diagnose PKD using imaging. If you’re 30-39 and have a family history, finding just 10 or more cysts on an ultrasound is enough to confirm ADPKD. For younger people or those without a family history, CT scans or MRIs give clearer pictures. Genetic testing is now widely available for around $1,200 and is recommended if you’re planning a family, have atypical symptoms, or were diagnosed young.
ARPKD is usually caught before or right after birth. Prenatal ultrasounds can show unusually large kidneys in a fetus. Newborns with ARPKD often have trouble breathing because their kidneys are so swollen they push on the lungs.
What Happens When Your Kidneys Fail?
Over time, the cysts grow, the kidneys swell-sometimes weighing up to 30 pounds-and function drops. About half of people with ADPKD will need dialysis or a transplant by age 60. For those with PKD1 mutations, that number can be even higher. By age 70, three out of four ADPKD patients will have reached kidney failure.
Once your kidneys fail, your body can’t clean your blood anymore. Dialysis takes over that job-either through a machine (hemodialysis) or a tube in your belly (peritoneal dialysis). But dialysis isn’t a cure. It’s a life-saver, but it’s exhausting. Many people on dialysis report constant fatigue, dietary restrictions, and long hours tied to machines.
Kidney transplant is the best long-term solution. A healthy kidney from a donor can restore near-normal function. But wait times vary. In the U.S., you might wait 3 to 5 years. Blood type and location matter a lot. In South Africa, access to transplants is even more limited, especially outside major cities.
How Is It Managed Today?
There’s no cure yet. But we can slow it down-and that makes a huge difference.
Control your blood pressure. This is the single most important thing you can do. Target: below 130/80 mmHg. For some, even tighter control (below 110/75) can slow cyst growth by 14%. ACE inhibitors or ARBs are the go-to medications. One patient in the American Kidney Fund community started treatment at 28 and kept their kidney function at 65% at age 45-despite having a strong family history.
Take tolvaptan (Jynarque). This is the first drug approved specifically to slow ADPKD progression. It works by blocking a hormone that makes cysts grow. In clinical trials, it reduced kidney function decline by 1.3 mL/min per year. But it’s expensive-over $115,000 a year in the U.S.-and can cause serious side effects like liver damage. It’s only for people with rapidly progressing disease, confirmed by imaging and lab tests.
Watch your diet and fluids. Avoid excessive salt, processed foods, and high-protein diets. Stay well-hydrated. Some studies suggest drinking 3 liters of water a day may help slow cyst growth by suppressing vasopressin, the same hormone tolvaptan blocks.
Manage pain and infections. Chronic pain affects 78% of PKD patients. Over-the-counter painkillers like acetaminophen are safer than NSAIDs (ibuprofen, naproxen), which can hurt your kidneys. Kidney infections need quick antibiotics-delayed treatment can lead to permanent damage.
What’s New in Research?
The field is moving fast. In 2024, new drugs like lixivaptan and bardoxolone methyl are in late-stage trials. Bardoxolone showed a 4.9 mL/min improvement in kidney function over placebo in a 2022 study. These aren’t cures, but they could mean years of extra healthy kidney life.
Gene therapy is still years away, but researchers are mapping how the PKD1 and PKD2 genes go wrong at the cellular level. The goal? To fix the root problem, not just slow the damage.
Genetic testing is becoming more routine. If you’re 25 and your dad had PKD, getting tested now lets you plan ahead-start blood pressure meds early, avoid risky jobs, consider family planning options.
Living With PKD: The Human Side
It’s not just about labs and scans. The emotional toll is real. In a 2023 survey by the PKD Foundation, 63% of patients said they lived with anxiety about kidney failure. One Reddit user wrote: “It took seven years and three doctors before I got diagnosed-even though my dad had it.”
Chronic pain is the #1 complaint. Many describe it as a constant dull ache that flares up after physical activity or during infections. Sleep suffers. Work becomes harder. Relationships strain under the weight of uncertainty.
But there are success stories. People who start managing their blood pressure early, stay active, and join support groups report better quality of life. One woman in her 40s told her group: “I didn’t know I could still hike, travel, and work full-time with PKD-until I started taking control.”
Costs and Challenges
PKD isn’t just a health issue-it’s a financial one. In the U.S., annual costs for ADPKD average $45,300. In the year before dialysis, that jumps to $95,700. Even with insurance, co-pays for tolvaptan can be $5,000 a month. In countries without universal healthcare, many go without treatment.
And while PKD only causes 2% of kidney failure cases, it eats up 5% of Medicare’s ESRD budget. Why? Because patients are younger. They need treatment for decades, not just a few years.
What Can You Do Today?
- If you have a family history of PKD, get screened-even if you feel fine.
- Get your blood pressure checked at least once a year. If it’s above 130/80, talk to your doctor about ACE inhibitors or ARBs.
- Drink plenty of water. Avoid soda and excessive caffeine.
- Stay active. Walking, swimming, yoga-low-impact movement helps.
- Join a support group. You’re not alone. The PKD Foundation and local nephrology clinics offer resources.
- If you’re planning a family, consider genetic counseling.
Final Thoughts
Polycystic kidney disease is not a death sentence. It’s a lifelong condition, yes-but with early detection and smart management, you can live well for decades. The tools are here: better drugs, smarter monitoring, stronger support. The key is acting before the damage becomes irreversible. If you or someone you love has PKD, don’t wait for symptoms to get worse. Start now. Your kidneys will thank you.






It's wild how something so genetic can feel so personal. I've watched my uncle go from hiking every weekend to needing dialysis in five years. The cysts don't just grow-they steal your future, one milliliter at a time. And yet, people act like it's just another chronic condition. It's not. It's a slow-motion eviction from your own body.
I just want to say to anyone reading this: you're not alone. I was diagnosed at 29, and I thought my life was over. But I started walking daily, switched to water instead of soda, and joined a local PKD group. I'm 37 now, still working full-time, and just got back from a trip to Costa Rica. It's hard, but it's not the end. There's still joy here.
Honestly, it's a bit embarrassing how little the medical community does for PKD patients. We're talking about a disease that affects 1 in 1,000 people, yet tolvaptan costs more than a luxury SUV. Meanwhile, Big Pharma is out here developing five new weight-loss drugs that do nothing but make people jittery. The system is broken. And no, I'm not just mad because my insurance denied my prescription. I'm mad because it's systemic.
So let me get this straight-you're telling me drinking 3 liters of water slows down cyst growth? That's it? No magic pill, no gene edit, just H2O? And you expect people to believe this is science? My cousin drank a gallon a day for ten years and still got a transplant at 48. This feels like placebo medicine dressed up in lab coats.
I read this whole thing and just cried. My sister has PKD and she never talks about it. She says she doesn't want to 'burden' anyone. But I see her wincing when she stands up. I see her skipping birthday dinners because she's too tired. I wish she knew how much it helps just to say it out loud. You're not a burden. You're a person. And you deserve to be heard.
For anyone considering genetic testing: do it. Even if you're asymptomatic. I got tested at 22 because my dad had PKD. Turned out I had PKD2. Started on an ARB at 24. My GFR is still at 78 at 31. Early intervention isn't glamorous, but it's the difference between living and just existing. Also, avoid NSAIDs like the plague. Seriously.
I'm so sorry you're going through this 😭 I know exactly how it feels. My brother died at 22 from ARPKD. I've been waiting for a transplant for 7 years and they keep saying 'not urgent enough'. I just want to live. Why is this so hard? 😔
It is truly remarkable, if not somewhat astonishing, how the biomedical community has, over the past decade, managed to shift the paradigm of PKD management from mere palliative care to proactive, disease-modifying intervention. One must acknowledge, however, that the economic burden placed upon individuals in nations without universal healthcare is nothing short of catastrophic. I have, for instance, observed that the cost of tolvaptan, while exorbitant, is in fact reflective of the R&D investment required to bring such a targeted therapy to market. That said, access remains deeply inequitable. One cannot help but wonder if the pharmaceutical industry's pricing models are truly aligned with the public good.
I have PKD too and i live in india. no one here knows about it. my doctor said its just 'kidney problem'. i dont have money for tolvaptan. i drink water and try to rest. i feel bad for my kids. they might get it too. but i still laugh with them every day. 🙏
I just want to say thank you to everyone who shared their story. It’s not easy to open up like this. I’ve been silent for years too. But reading this made me realize I don’t have to carry it alone anymore. I’m going to call my doctor tomorrow about getting screened. And if anyone wants to chat, I’m here. No judgment. Just listening.
Everyone's acting like this is some heroic battle. Newsflash: you're not a warrior. You're a patient. And most of you are just doing what you're told by doctors who don't even understand your life. I've seen too many people waste their 30s chasing 'lifestyle hacks' while their kidneys turn to mush. Wake up.
I'm a nephrologist in Delhi. I treat PKD patients daily. The biggest challenge isn't the disease-it's the lack of awareness. Families don't know to screen. Doctors don't know to test. We've had patients come in with stage 5 CKD and no idea why. Early detection saves kidneys. And kidneys save lives. If you have a family history, get an ultrasound. It takes 20 minutes. It could change everything.
ADPKD: autosomal dominant, PKD1/2 mutations, cystogenesis via cilia dysfunction, vasopressin-mediated fluid secretion. Tolvaptan = V2R antagonist. GFR decline = 2.5 mL/min/yr baseline; tolvaptan reduces it by 1.3. Number needed to treat for 5-year delay in ESRD = 7.3. Insurance denies it? Then appeal with the TEMPO 3:4 data. Done.
I'm from the UK and we've got the NHS, so we get tolvaptan if you qualify. But the wait for transplant is 3 years minimum. My mate had his in 2022. He says the hardest part wasn't the surgery-it was the loneliness. No one gets it until they're in it. If you're reading this and you're scared? You're allowed to be. Just don't stay quiet.
So let me get this straight-you're telling me a guy in India drinks water and laughs with his kids while someone in America is paying $5k/month for a pill that makes their liver scream? And we're supposed to feel inspired? This isn't hope. This is capitalism with a kidney-shaped hole in it.