When gabapentin and pregabalin were first approved for seizures and nerve pain, doctors saw them as safe alternatives to opioids. But over the last decade, the picture has changed. Today, these drugs - known as gabapentinoids - are among the most prescribed medications for chronic pain, yet they carry serious risks that many patients and even some providers still underestimate. The real danger isn’t just the pain they treat - it’s what happens when dosing goes too high, when dizziness isn’t taken seriously, and when misuse slips under the radar.
How Gabapentinoids Are Actually Dosed - And Why More Isn’t Better
There’s a myth that higher doses of gabapentin or pregabalin mean better pain control. That’s not true. The gabapentin dosing range for neuropathic pain is 900 mg to 3,600 mg daily, split into three doses. But here’s what the data shows: patients taking more than 1,800 mg per day get almost no extra pain relief - yet their risk of dizziness, falls, and confusion jumps sharply.
The FDA and the American Academy of Neurology both agree: doses above 1,800 mg daily offer diminishing returns. A 2023 review of 12 clinical trials found that patients on 1,800 mg daily had the same pain reduction as those on 3,600 mg - but with half the side effects. That’s why experts now recommend starting low: 100-300 mg once daily, then increasing by no more than 300 mg every 3 to 7 days. For older adults, especially those over 70, many clinicians now cap doses at 900 mg daily - even if pain persists.
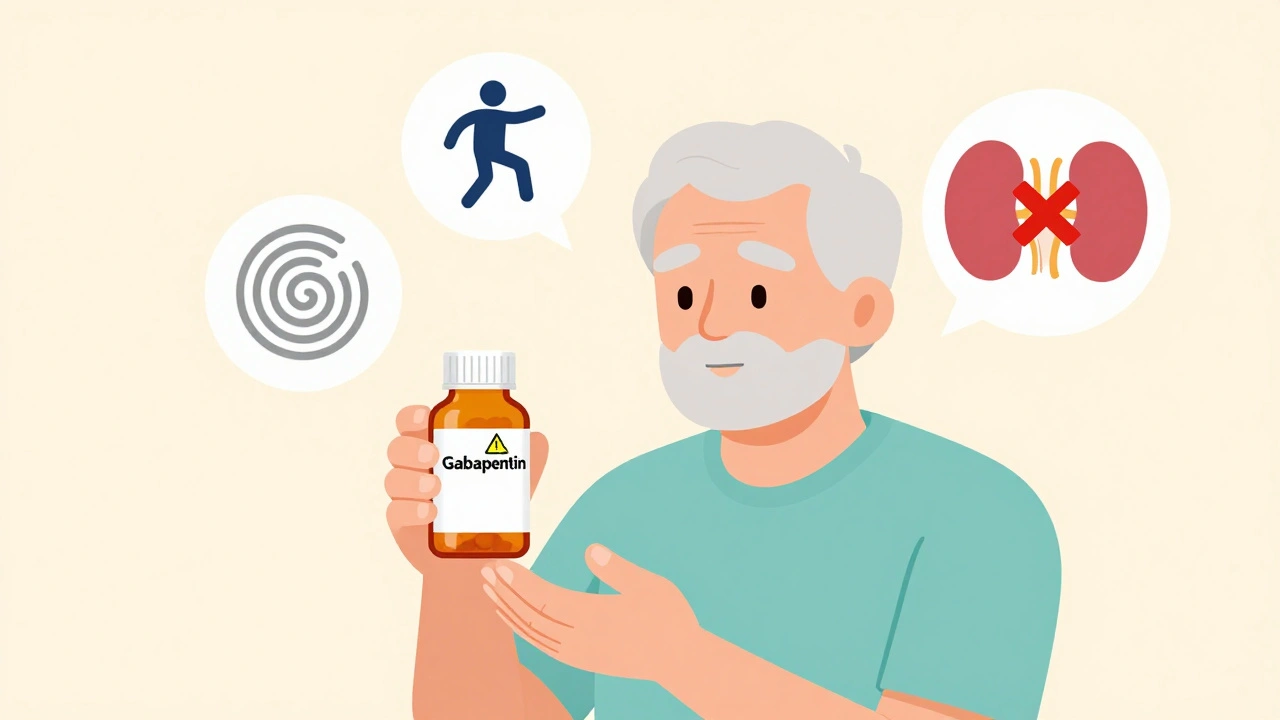
Renal function changes everything. If your kidneys aren’t filtering well, gabapentin builds up in your system. For someone with a creatinine clearance under 30 mL/min, the max daily dose should be 600 mg or less. Yet many prescriptions ignore this. A 2022 study in Journal of Pain Medicine found that nearly 40% of elderly patients on gabapentin had no kidney function check in the past year. That’s not just careless - it’s dangerous.
Dizziness Isn’t Just an Annoyance - It’s a Fall Risk
Dizziness is the most common side effect of gabapentinoids. It’s not rare. It’s expected. Clinical trials show 20-30% of patients feel dizzy, but in real life, it’s worse. On Reddit’s pain forums, 78% of users reported dizziness as their top reason for stopping the drug. In patients over 65, the rate climbs to over 40%. And for those with balance problems or vertigo? It can be 50% or higher.
What makes dizziness so dangerous isn’t just the spinning feeling - it’s the timing. Most cases happen during the first week of dose increases. That’s when your brain is still adjusting. And if you take gabapentin at night, the dizziness can linger into the morning, making it hard to get out of bed safely. That’s why the American Geriatrics Society warns: never give gabapentinoids to frail older adults without a fall risk assessment.
One 74-year-old woman in Georgia started on 300 mg three times daily for diabetic neuropathy. Within five days, she fell twice in her kitchen. Her doctor didn’t realize the connection until she mentioned the timing. Her dose was cut to 900 mg daily - and her dizziness disappeared. She didn’t lose pain control. She just stopped nearly breaking her hip.
Prevention is simple but often ignored: start slow, avoid evening doses if possible, and check for dizziness every week during titration. If a patient says they feel lightheaded, don’t just say, “It’ll pass.” That’s not care - that’s dismissal.

Misuse Is Real - And It’s Growing
When people talk about opioid misuse, gabapentinoids rarely come up. But they should. Between 2012 and 2020, deaths involving gabapentin increased by nearly 500%. Why? Because many people with opioid use disorder use gabapentin to boost the high or ease withdrawal. A 2022 study in Addiction found that 15-22% of people in opioid treatment programs deliberately took gabapentin in high doses - often 3,600 mg or more - to get a sedated, euphoric feeling.
It’s not just street use. Prescription misuse is common. Patients who aren’t addicted may still take extra pills because they think it helps their sleep or anxiety. One patient in Michigan told his doctor he was taking 4,800 mg daily because “it makes me feel calm.” He didn’t have nerve pain. He had anxiety. He was self-medicating. He ended up in the ER after passing out in the shower.
The FDA added misuse warnings to gabapentin labels in 2019. Since then, 49 U.S. states have put gabapentin on their prescription drug monitoring programs (PDMPs). That means pharmacists can now see if someone is getting it from multiple doctors. But many providers still don’t check the PDMP before prescribing.
Here’s what works: screen everyone for substance use before starting gabapentin. Ask directly: “Have you ever used prescription meds for reasons other than how they were prescribed?” If the answer is yes - or even if you’re unsure - consider alternatives. And if you do prescribe it, use short initial scripts - no more than a 7-day supply - especially for acute pain.
What Safe Prescribing Looks Like in Practice
Safe gabapentinoid use isn’t about avoiding them. It’s about using them wisely. The American Medical Association’s new “START” protocol gives a clear roadmap:
- Screen for kidney function and substance use history before prescribing.
- Titrate slowly - increase by 300 mg or less every 3-7 days, never faster.
- Assess for dizziness, confusion, or unsteadiness every week during the first month.
- Review every month: Is this still helping? Are side effects worse than the pain?
- Taper if stopping - never quit cold turkey. Reduce by 300 mg every 3 days to avoid withdrawal seizures or severe anxiety.
For elderly patients, the rules are stricter. The Beers Criteria says: don’t start anyone over 80 on more than 900 mg daily. And if they’re already on it, consider cutting the dose - even if they’ve been on it for years. Many older adults don’t need high doses to feel relief. They just need the right one.
Pharmaceutical companies are working on abuse-deterrent versions. Pfizer’s extended-release gabapentin XR, expected in mid-2024, is designed to prevent crushing or dissolving for injection. But until those are widely available, the best deterrent is careful prescribing.

When to Stop - And What to Try Instead
Not every patient needs gabapentinoids. Many have pain that responds better to physical therapy, cognitive behavioral therapy, or non-opioid options like duloxetine or topical capsaicin. Gabapentinoids work best for nerve pain - burning, shooting, electric sensations - not general aches or arthritis.
If you’ve been on gabapentin for more than 3 months and aren’t sure it’s helping, ask yourself: Am I taking it because it works - or because I’m afraid of stopping? Withdrawal symptoms like insomnia, anxiety, or nausea are real, but they’re manageable with a slow taper. Most patients who taper over 2-4 weeks feel better than they expected.
And if you’re taking more than 1,800 mg daily? That’s a red flag. You’re not getting more pain relief - you’re just increasing your risk of dizziness, falls, and dependence. Talk to your doctor about lowering your dose. You might be surprised how much better you feel.
The data is clear: gabapentinoids can help - but only if used with caution. They’re not magic pills. They’re tools. And like any tool, they can hurt as much as they heal if misused.
Can gabapentin cause dizziness even at low doses?
Yes. While dizziness is more common at higher doses, some people experience it even at 300 mg daily, especially older adults or those with inner ear issues. It’s not about the dose alone - it’s about individual sensitivity. If you feel lightheaded, even on a low dose, tell your doctor. Don’t assume it’s normal.
Is pregabalin safer than gabapentin?
Not necessarily. Pregabalin is more potent and absorbed faster, so it can cause dizziness and misuse more easily than gabapentin at equivalent doses. Both carry similar risks. Pregabalin’s higher bioavailability means even small increases in dose can lead to bigger side effects. Neither is inherently safer - both require careful dosing.
Can I drink alcohol while taking gabapentin?
No. Alcohol increases dizziness, drowsiness, and the risk of falls when combined with gabapentinoids. It can also raise the chance of respiratory depression, especially at higher doses. Even one drink can make you unsteady. Avoid alcohol completely while on these medications.
What happens if I stop gabapentin suddenly?
Stopping abruptly can cause withdrawal symptoms including anxiety, insomnia, nausea, sweating, and in rare cases, seizures. The FDA recommends reducing the dose by 300 mg every 3 days. If you’ve been on a high dose for months, tapering over 2-4 weeks is safest. Never quit without medical supervision.
Are there natural alternatives to gabapentin for nerve pain?
Yes. Topical capsaicin cream, acupuncture, physical therapy, and certain supplements like alpha-lipoic acid or magnesium have shown benefit in clinical studies for neuropathic pain. Cognitive behavioral therapy (CBT) is also effective for managing chronic pain without medication. These aren’t instant fixes, but they’re safer long-term options - especially for older adults or those with a history of substance use.
What to Do Next
If you’re on gabapentin or pregabalin and haven’t had a kidney test in over a year - get one. If you’re taking more than 1,800 mg daily and still have pain - talk to your doctor about lowering the dose. If you’ve ever taken extra pills to feel calmer or sleep better - be honest with your provider. You’re not alone. And you don’t have to keep taking risks.
The goal isn’t to scare you off these medications. It’s to make sure you’re using them safely - so you get relief without the hidden dangers. Dizziness isn’t just a side effect. Misuse isn’t just a statistic. These are real risks with real consequences. The good news? With the right approach, you can still manage your pain - without putting your safety at risk.






i just started gabapentin last week for my sciatica and already feel like a zombie at night lol. my dr said itll pass but im not sure i believe him.
As a neurologist who’s managed over 200 patients on gabapentinoids, I can confirm the 1,800 mg ceiling is evidence-based. The pharmacokinetics are clear: beyond that threshold, plasma concentration plateaus while CNS side effects escalate linearly. What’s more alarming is how often renal function is overlooked-especially in geriatric populations where creatinine clearance declines with age. I routinely screen eGFR before initiating therapy and cap doses at 900 mg for patients over 70 unless they have normal renal function. The myth of ‘more is better’ persists because patients report subjective relief, but objective measures show no additional analgesia. Always prioritize safety over perceived efficacy.
my buddy was on 3600mg for years and said it helped his anxiety but then he started blacking out in the shower. he finally got tapered down to 900mg and says he feels like himself again. no more dizziness, no more fog. i wish more docs would listen instead of just writing scripts. also-alcohol? nope. not even one beer. it’s a recipe for a fall.
It is worth noting that the FDA’s 2019 labeling update regarding misuse potential was a significant regulatory milestone, yet implementation remains inconsistent across prescribing practices. The adoption of prescription drug monitoring programs (PDMPs) has been uneven, with rural providers less likely to integrate them into clinical workflows. Furthermore, the absence of standardized screening protocols for substance use history prior to gabapentinoid initiation contributes to underdetection of misuse. A prospective cohort study conducted in 2021 demonstrated that clinicians who employed structured substance use questionnaires reduced high-dose prescriptions by 37% over six months. This suggests that behavioral interventions, not just pharmacological ones, are essential to mitigating risk.
I have seen too many elderly patients on gabapentin-some for over a decade-prescribed without a single follow-up. Their balance deteriorates. Their cognition fades. And when families ask why, the answer is always, ‘It was working fine.’ But ‘fine’ isn’t safe. The Beers Criteria exists for a reason. We are not doing our duty when we allow chronic high-dose gabapentinoid use in frail older adults. It’s not just negligence-it’s institutionalized harm disguised as compassion. We need mandatory kidney panels, mandatory fall risk assessments, and mandatory monthly reviews. Not suggestions. Requirements.
lol so now we’re treating gabapentin like it’s heroin? next they’ll make us sign a waiver just to get a headache pill. my grandma takes it for her legs and she’s fine. stop scaring people with stats. also, alcohol? i drink wine with mine. no big deal.
Oh great. Another post that sounds like it was written by a pharmacist who’s never met a patient who actually suffers. You want us to stop gabapentin? Try telling that to someone with 10 years of diabetic neuropathy who’s tried everything else. CBT? Capsaicin? You think I’m gonna rub chili on my feet instead of taking something that lets me walk? The real problem isn’t the drug-it’s that we don’t have better options. So yes, I’ll take my 2400 mg and my dizziness. At least I can get out of bed.
Wow. So now doctors are supposed to be mind readers? You want us to screen for substance abuse before prescribing? What next-background checks? And who’s gonna pay for all these ‘mandatory’ tests? This is America, not Sweden. People need relief. Not lectures.