Desvenlafaxine Interaction Checker
Check Medication Interactions
Enter any prescription, OTC, or herbal medication to see if it interacts with desvenlafaxine.
When you’re prescribed Desvenlafaxine is a serotonin‑norepinephrine reuptake inhibitor (SNRI) used to treat major depressive disorder. It works by increasing the levels of serotonin and norepinephrine in the brain, helping to lift mood and improve energy. the last thing you want is a surprise side effect from another drug. Below is a practical roadmap that tells you which medicines you should keep away from while on desvenlafaxine.
Key Takeaways
- Avoid combining desvenlafaxine with monoamine oxidase inhibitors (MAO‑Is) - it can trigger serotonin syndrome.
- NSAIDs, aspirin, and warfarin raise bleeding risk when taken together.
- Drugs that affect CYP2D6 (like fluoxetine or quinidine) can raise desvenlafaxine levels and increase side‑effects.
- Tramadol, linezolid, and lithium each have special cautions because of overlapping neurotransmitter pathways.
- Always tell your prescriber about over‑the‑counter meds, supplements, and herbal products.
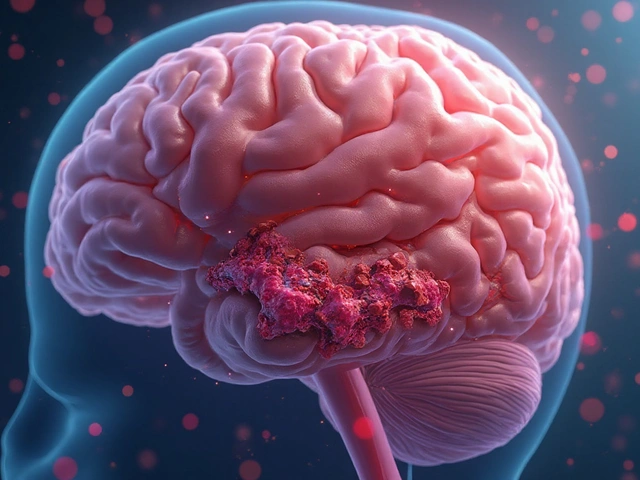
How Desvenlafaxine Works
Desvenlafaxine blocks the reuptake pumps for serotonin and norepinephrine, allowing more of these chemicals to stay active in the synaptic cleft. The result is better mood regulation and reduced anxiety for many patients. Because it influences two neurotransmitters, the drug sits at the crossroads of several metabolic pathways, making it a prime candidate for interactions.
Why Interactions Matter
Even a modest interaction can tip the balance from therapeutic to toxic. For example, raising serotonin too high can cause agitation, fever, rapid heart rate, and in severe cases, serotonin syndrome a potentially life‑threatening condition marked by neuromuscular hyperactivity, autonomic instability, and altered mental status.. On the other side, reduced clearance of desvenlafaxine can amplify common side‑effects like nausea, insomnia, and hypertension.

Major Medication Classes to Avoid
Below is a quick scan of drug families that commonly clash with desvenlafaxine.
| Medication Class | Interaction Type | Clinical Consequence | Recommended Action |
|---|---|---|---|
| Monoamine Oxidase Inhibitors (MAO‑Is) | Pharmacodynamic - additive serotonin increase | Serotonin syndrome | Discontinue MAO‑I at least 14 days before starting desvenlafaxine |
| Selective Serotonin Reuptake Inhibitors (SSRIs) & other SNRIs | Pharmacodynamic - serotonin excess | Serotonin syndrome, heightened side‑effects | Avoid concurrent use unless under strict specialist supervision |
| Non‑steroidal Anti‑Inflammatory Drugs (NSAIDs) / Aspirin | Pharmacodynamic - platelet inhibition | Increased risk of GI bleeding | Prefer acetaminophen for mild pain; monitor for signs of bleeding |
| Warfarin & other anticoagulants | Pharmacodynamic - enhanced anticoagulation | Bleeding complications | Check INR more frequently; consider dose adjustment |
| CYP2D6 inhibitors (e.g., fluoxetine, quinidine) | Pharmacokinetic - reduced metabolism | Elevated desvenlafaxine levels → hypertension, tachycardia | Switch to a non‑CYP2D6 inhibitor or lower desvenlafaxine dose |
| Tramadol | Pharmacodynamic - serotonergic and opioid overlap | Serotonin syndrome, respiratory depression | Avoid or use lowest effective dose with close monitoring |
| Linezolid (antibiotic) | Pharmacodynamic - MAO inhibition | Serotonin syndrome | Choose alternative antibiotic when possible |
| Lithium | Pharmacodynamic - neurochemical interaction | Tremor, confusion, potential toxicity | Monitor lithium levels closely; adjust dose if needed |
Specific High‑Risk Drugs
Fluoxetine is a potent CYP2D6 inhibitor. When taken with desvenlafaxine, it can push the latter’s blood concentration up by 30‑50 percent. Patients often report intensified jitteriness or a spike in blood pressure.
Tramadol is both a weak opioid and a serotonin‑norepinephrine reuptake inhibitor. Combined use has been linked to case reports of serotonin syndrome, especially in older adults.
Linezolid acts like a reversible MAO inhibitor. Even a short 5‑day course can precipitate serious serotonin excess if you’re on desvenlafaxine.
Lithium can amplify tremor and confusion. Since both drugs affect the central nervous system, regular lithium level checks become mandatory.
Warfarin doesn’t change desvenlafaxine levels but can make bleeding more likely. If you’re on a stable INR, adding desvenlafaxine may push you into the therapeutic range of over‑anticoagulation.
Managing Interaction Risks
Here’s a step‑by‑step checklist you can use when starting or adjusting desvenlafaxine therapy:
- List every prescription, OTC, herbal supplement, and vitamin you currently take.
- Identify any drugs from the interaction table above.
- Talk to your prescriber about safer alternatives (e.g., acetaminophen instead of ibuprofen for mild aches).
- If a high‑risk drug can’t be stopped, ask for a baseline lab panel - CBC, liver enzymes, INR, and lithium level if applicable.
- Schedule a follow‑up within 2‑4 weeks to review side‑effects and adjust dose.
- Stay alert for red‑flag symptoms: sudden fever, sweating, confusion, fast heart beat, or unusual bruising. Call your doctor immediately if they appear.
Keeping a written medication list in your wallet can save you time during emergencies.
Special Populations
Older adults often take multiple drugs for chronic conditions, putting them at higher interaction risk. Dose‑adjust desvenlafaxine to 25 mg daily if you’re over 65 and monitor blood pressure weekly.
Pregnant or breastfeeding women should discuss risks with an obstetrician because serotonin‑modulating drugs can affect fetal neurodevelopment. Generally, the benefits of treating severe depression outweigh potential risks, but alternative therapies might be preferred.
Patients with liver impairment may experience slower clearance. In such cases, start at the lowest possible dose and check plasma levels when available.
Frequently Asked Questions
Can I take ibuprofen with desvenlafaxine?
Occasional ibuprofen at low doses is usually okay, but regular use raises bleeding risk. Stick to acetaminophen for everyday pain if possible.
Do herbal supplements interact with desvenlafaxine?
St. John’s wort is a strong CYP450 inducer and can lower desvenlafaxine levels, making it less effective. Avoid it or discuss dose changes with your doctor.
What signs indicate serotonin syndrome?
Look for agitation, rapid heartbeat, high fever, muscle rigidity, and dilated pupils. If you notice a cluster of these symptoms, seek emergency care.
Is it safe to combine desvenlafaxine with nicotine replacement therapy?
Nicotine patches or gum don’t affect serotonin pathways, so they’re generally safe. However, monitor blood pressure, as both nicotine and desvenlafaxine can raise it.
How long should I wait after stopping an MAO‑I before starting desvenlafaxine?
A minimum wash‑out period of 14 days is recommended to avoid serotonin syndrome. Some clinicians extend this to 21 days for safety.
Bottom Line
Desvenlafaxine can be a lifeline for depression, but it’s a bridge that other drugs can easily tip. By knowing which medication classes to steer clear of, checking doses, and staying alert for warning signs, you protect yourself from dangerous side‑effects while keeping the mood‑boosting benefits. Always keep the conversation open with your prescriber-your safety depends on it.






Ever notice how the drug companies keep the warning labels buried deep in the fine print? It's like they want us to think the only danger is the depression, not the cocktail of meds we might already be taking. When you add an SNRI like desvenlafaxine to a regimen that already includes an NSAID or a MAO‑I, you’re basically inviting a perfect storm. The more you trust the system, the more you expose yourself to hidden side‑effects.
Desvenlafaxine is primarily metabolized by CYP2D6, so any strong inhibitor of that enzyme-fluoxetine, quinidine, or even certain herbal extracts-can raise plasma concentrations by roughly a third. Elevated levels tend to manifest as hypertension, tachycardia, or intensified nausea. Conversely, in rapid metabolizers the drug may be cleared too quickly to achieve therapeutic effect. Adjusting the dose based on known CYP2D6 interactions is a standard clinical practice.
It is frankly irresponsible for anyone to casually combine powerful neuroactive agents without a thorough understanding of the underlying pharmacology. The premise that a patient can simply pick up a pack of ibuprofen and a prescription for desvenlafaxine and expect benign outcomes is a dangerous delusion. First, the serotonin–norepinephrine reuptake inhibition already raises the baseline neurotransmitter tone, which means adding another serotonergic drug pushes the system toward excess. That excess is not a trivial side effect; it can culminate in serotonin syndrome, a condition that can be fatal if not recognized promptly. Second, the inhibition of platelet aggregation by NSAIDs and the anticoagulant potentiation by warfarin are well‑documented, yet many prescribers ignore these interactions until bleeding occurs. Third, the cytochrome P450 system, particularly CYP2D6, is a common pathway for many psychiatric and cardiac medications, and neglecting its role leads to unpredictable plasma levels. Fourth, there is a moral obligation to inform patients about over‑the‑counter supplements like St. John’s wort, which can dramatically reduce drug efficacy. Fifth, clinicians must recognize that older adults often have polypharmacy and diminished renal clearance, amplifying these risks. Sixth, the legal ramifications of negligence in prescribing can be severe, ranging from malpractice claims to loss of licensure. Seventh, beyond the immediate physiological hazards, the psychological burden on patients who experience adverse events can erode trust in the healthcare system. Eighth, healthcare providers should proactively schedule follow‑up visits within two to four weeks after initiating therapy to monitor for emerging side effects. Ninth, a written medication list carried by the patient is not a suggestion but a necessity that can prevent emergency department mishaps. Tenth, when high‑risk drugs such as linezolid or tramadol must be used, the prescribing physician should document the justification and obtain informed consent. Eleventh, the responsibility does not end at the prescription pad; pharmacists play a critical role in double‑checking for interactions before dispensing. Twelfth, insurance formularies that limit medication choices should not become an excuse to overlook safety. Thirteenth, ongoing education for both clinicians and patients about drug–drug interactions is essential to maintain therapeutic efficacy. Fourteenth, any deviation from these safeguards betrays the principle of “do no harm.” Finally, the cumulative effect of ignoring these guidelines is a healthcare environment where preventable tragedies become commonplace, and that is a legacy no professional should accept.
Avoid mixing MAO‑Is with desvenlafaxine at all costs.
That warning reads like a courtroom subpoena, reminding us that shortcuts in medication safety are nothing short of criminal negligence.
I get how overwhelming all these warnings can feel, especially when you’re trying to manage depression alongside other health issues. It helps to break down the list into categories-bleeding risks, serotonin overload, metabolic interactions-and talk them over with your prescriber. Keeping a simple spreadsheet of your meds, dosages, and any noted side‑effects can turn chaos into clarity. Remember, you’re not alone in navigating this maze; your healthcare team is there to guide you every step of the way.
Many patients from different backgrounds may not realize that over‑the‑counter products like herbal teas can still affect drug metabolism so it’s worth asking about every supplement you take.
While it’s true that some supplements have mild effects, the bulk of evidence points to major drug classes as the real culprits for serious interactions.
It can be scary to think about all the possible drug combinations, but taking it one step at a time and staying in close contact with your doctor can make the process much less intimidating.
Start by writing down every prescription, over‑the‑counter pain reliever, and supplement you use. Then flag any items that appear in the interaction table-especially NSAIDs, warfarin, and CYP2D6 inhibitors. Bring that list to your next appointment and ask your doctor to review it with you. Small, systematic actions like this can prevent big problems down the road.
I’ve found that keeping that notebook in a pocket and updating it after each pharmacy visit really helps keep everything straight.
In accordance with best clinical practice, it is advisable to routinely assess bleeding risk and serotonergic load when initiating desvenlafaxine therapy, thereby ensuring optimal patient safety.
One might argue that such “best practice” recommendations are merely a veneer, designed to give the illusion of control while the pharmaceutical elite continue to profit from hidden adverse events.