Immunosuppressant Drug Interaction Checker
Check if your medications interact dangerously with azathioprine or mycophenolate. Based on FDA guidelines and clinical studies, this tool identifies critical interactions requiring dose adjustments or avoidance.
Interaction Results
When you’re on immunosuppressants after a transplant or for an autoimmune disease, the goal is simple: keep your immune system from attacking your new organ or your own body. But here’s the catch - these drugs don’t work in isolation. They interact with other medications, foods, and even your own genes. Two of the most commonly used drugs - azathioprine and mycophenolate - are powerful, but they come with hidden risks if not managed right.
How Azathioprine and Mycophenolate Work - and Why It Matters
Azathioprine has been around since the 1960s. It’s a prodrug, meaning your body turns it into 6-mercaptopurine, which then becomes toxic compounds that stop immune cells from multiplying. Think of it like cutting off the supply line to enemy soldiers. But here’s the twist: your liver uses an enzyme called TPMT to break it down. About 89% of people have normal TPMT activity. But 11% have less, and 0.3% have almost none. If you’re in that small group and take a standard dose, you’re at risk for life-threatening drops in white blood cells - think severe infections or even sepsis.
Mycophenolate, approved in the 1990s, works differently. It blocks an enzyme called IMPDH, which immune cells need to make DNA. Without that, they can’t multiply. It’s more targeted than azathioprine, which is why it’s now the go-to for most kidney transplants. But it’s not perfect. It’s absorbed poorly if taken with food or antacids. And if your kidneys aren’t working well, the inactive byproduct builds up and pushes more active drug into your bloodstream - raising your risk of side effects.
The Big Interaction: Allopurinol and Azathioprine
One of the most dangerous combinations is azathioprine with allopurinol. Allopurinol is often given to gout patients to lower uric acid. But when taken with azathioprine, it shuts down the main way your body clears the drug. This causes thioguanine nucleotides to pile up - sometimes to 3.5 times normal levels. The result? A 6.3-fold increase in severe bone marrow suppression. That’s not a minor side effect. It’s a medical emergency. The FDA has a black box warning for this. If you’re on azathioprine and your doctor prescribes allopurinol, push back. Ask if there’s an alternative. If not, your azathioprine dose must be cut by 75% - and even then, close monitoring is non-negotiable.
Mycophenolate and Proton Pump Inhibitors (PPIs)
Mycophenolate needs an acidic environment in the stomach to be absorbed properly. That’s where PPIs like omeprazole or pantoprazole become a problem. These drugs reduce stomach acid, and that cuts mycophenolate absorption by 25-35%. In lupus nephritis patients, this can mean the drug doesn’t work well enough - leading to flare-ups or even kidney rejection. A Johns Hopkins study found that patients on PPIs had lower MPA levels and higher rates of disease activity. The fix? Either stop the PPI, switch to an H2 blocker like famotidine, or increase the mycophenolate dose. But never do this without checking blood levels.
Cyclosporine and Tacrolimus: The Transplant Triangle
Most transplant patients take a combo of drugs. Cyclosporine and tacrolimus are calcineurin inhibitors that work alongside azathioprine or mycophenolate. But here’s the tricky part: cyclosporine reduces mycophenolate exposure by 35-50%. Why? It blocks the enterohepatic recirculation - the process where mycophenolate gets recycled back into the bloodstream from the gut. If you switch from cyclosporine to tacrolimus, your mycophenolate levels can suddenly spike. Many patients don’t realize this until they’re hospitalized for diarrhea or low white blood cell counts. The solution? Monitor MPA levels when switching. Most transplant centers now check MPA AUC (area under the curve) - target is 30-60 mg·h/L. If you’re above that, reduce the dose. If you’re below, you’re at risk for rejection.
Azathioprine vs Mycophenolate: Efficacy and Side Effects
Let’s cut through the noise. Which one is better? It depends on what you need.
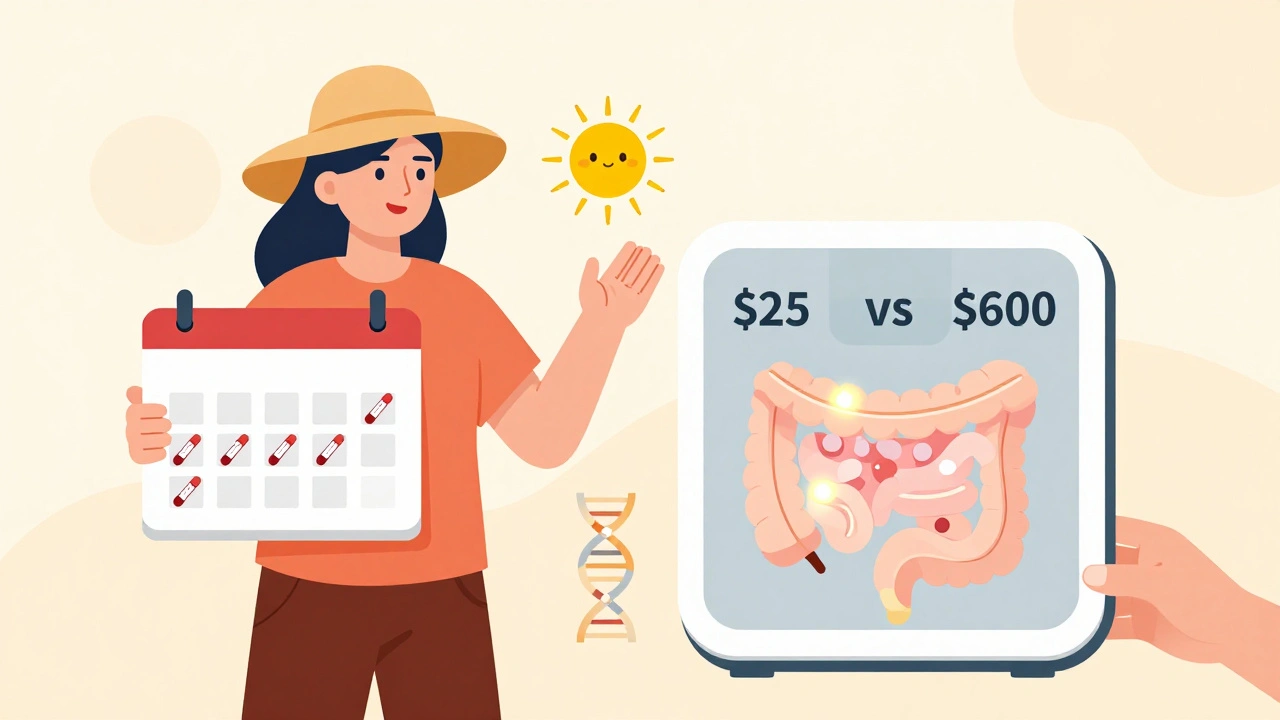
- Autoimmune hepatitis: Mycophenolate gets you into remission 68% of the time. Azathioprine? Only 46%. That’s a huge difference.
- Lupus nephritis: In the ALMS trial, mycophenolate led to complete kidney response in 56% of patients. Azathioprine? 42%.
- Side effects: Mycophenolate causes diarrhea in 30-40% of people. Azathioprine causes nausea and vomiting in 15-20%, but it’s more likely to cause sun sensitivity - severe burns from minor exposure. One patient in Durban told me he got a second-degree sunburn just walking to his car on a cloudy day.
- Bone marrow suppression: Azathioprine is worse here. Mycophenolate causes fewer low blood counts, which is why it’s preferred for younger patients.
- Cancer risk: Azathioprine carries a 1.8-fold higher risk of lymphoma and skin cancer. Long-term transplant recipients on azathioprine need annual skin checks.
- Cost: Azathioprine generics cost about $25 a month. Mycophenolate? Around $600. That’s why it’s still used in low-resource settings - and why some patients stop taking it.
What Patients Actually Experience
Real people don’t read clinical trials. They live with the side effects.
On transplant forums, 68% of users say they tolerate mycophenolate better than azathioprine - mostly because they don’t need as many blood tests. But 45% say the diarrhea is so bad they have to cut their dose. One woman in Texas switched from standard mycophenolate to the enteric-coated version (EC-MPS) and went from 5 bathroom trips a day to 1. Another man in South Africa couldn’t afford mycophenolate and stayed on azathioprine - he developed a skin cancer on his nose three years later.
Compliance is another issue. At 12 months, 82% of mycophenolate users are still taking it. Only 76% of azathioprine users are. Why? Cost. Many patients skip doses because they can’t afford it. Others forget because they have to take it twice a day on an empty stomach. That’s harder than it sounds.
Testing and Monitoring - What You Really Need
For azathioprine, you need a TPMT test before you even take your first pill. It’s not optional. It’s a blood or saliva test that costs $250-$400. If your TPMT is low, your dose must be cut by 75-90%. Many clinics now use genetic testing to predict this before prescribing. If you don’t get tested, you’re gambling with your life.
For mycophenolate, you don’t always need routine blood level checks - but you should if you’re on PPIs, have kidney problems, or are switching drugs. The MPA AUC test isn’t available everywhere, but it’s standard in transplant centers. If your level is below 30 mg·h/L, your risk of rejection goes up. Above 60, your risk of infection or low blood counts spikes.
And yes - you need to avoid multivalent ions. That means calcium, iron, magnesium, and aluminum. So no antacids, no iron pills, no multivitamins within two hours of taking mycophenolate. If you take them together, absorption drops by 25%.
What’s Changing Right Now
There’s new hope on the horizon. In 2023, a new delayed-release version of mycophenolate (Myfortic DR) hit the market. It’s designed to release the drug farther down the gut, where it’s better absorbed and less irritating. Early trials show 28% fewer GI side effects. That’s huge for patients who’ve given up on the drug because of nausea and diarrhea.
Also, the FDA approved a TPMT genotype-guided dosing calculator in 2022. It’s now used in 60% of U.S. transplant centers. It tells you exactly how much azathioprine to give based on your genes. That’s cut cytopenias by 37% in early adopters.
But here’s the reality: azathioprine isn’t disappearing. It’s still used in inflammatory bowel disease, where mycophenolate only works in 35% of cases. And in places like rural India or parts of Africa, it’s the only affordable option. Cost matters. Access matters. Sometimes, the best drug is the one you can actually get.
Final Takeaways - What to Do Now
- If you’re on azathioprine, confirm you had a TPMT test. If not, ask for one now.
- If you’re on mycophenolate and take a PPI, talk to your doctor about switching or adjusting your dose.
- If you’re on cyclosporine and your doctor wants to switch you to tacrolimus, ask for an MPA level check before and after.
- Avoid allopurinol completely if you’re on azathioprine - unless your doctor adjusts your dose and monitors you closely.
- Take mycophenolate on an empty stomach. Wait two hours after eating. Wait two hours before taking antacids or iron.
- Check your skin monthly for new moles or sores. Azathioprine increases skin cancer risk.
- Don’t skip doses because of cost. Ask about patient assistance programs. Many drugmakers offer them.
These drugs save lives. But they’re not simple. They require attention, testing, and communication with your care team. The difference between success and disaster often comes down to one question you didn’t ask - or one test you skipped.
Can I take azathioprine and mycophenolate together?
While some studies show the combination is safe in lupus patients who failed single-agent therapy, most transplant centers avoid it. Both drugs suppress bone marrow, and combining them increases infection and anemia risk. If used, it’s only under close supervision with weekly blood tests. Never start both without your doctor’s explicit plan.
Why does mycophenolate cause diarrhea?
Mycophenolate affects rapidly dividing cells - including those lining your gut. This leads to inflammation and reduced absorption, causing watery stools. Up to 40% of users experience it. Switching to the enteric-coated version (EC-MPS) or taking it with a small amount of food (if approved by your doctor) can help. Loperamide may be used short-term, but it doesn’t fix the root cause.
Is azathioprine still used in transplants today?
Yes, but only in about 15% of solid organ transplants. Mycophenolate is preferred because it’s more effective and has fewer bone marrow side effects. Azathioprine remains in use where cost is a barrier, or for specific conditions like inflammatory bowel disease, where it outperforms mycophenolate.
Do I need to avoid sunlight if I’m on azathioprine?
Absolutely. Azathioprine increases your skin’s sensitivity to UV light, raising your risk of squamous cell carcinoma and melanoma. Wear broad-spectrum SPF 50+ daily, even on cloudy days. Cover up. Avoid tanning beds. Get a full-body skin check every year.
How often should my blood be checked on these drugs?
For azathioprine, check CBC weekly for the first month, then monthly for three months, then every 2-3 months. For mycophenolate, check CBC and kidney function monthly for the first three months, then every 2-3 months. If you’re on PPIs, have kidney disease, or switched immunosuppressants, check more often - every 1-2 weeks until stable.






Of course the FDA's black box warning is just a distraction - real power players know that pharmaceutical companies engineer these interactions to keep you dependent. TPMT testing? That's a profit-driven scam. The real issue is that the WHO and Big Pharma colluded to phase out azathioprine because it's too cheap to control the market. You think your 'MPA levels' are being monitored for your safety? Nah. They're tracking your compliance so they can upsell you the $600 version. Wake up.
OMG I CANT BELIEVE THIS!! I WAS ON AZATHIOPRINE AND TOOK ALLOPURINOL FOR A WEEK AND DIDNT DIE??!! I THOUGHT I WAS GONNA GET SEPTIC OR SOMETHING!! MY DOCTOR JUST SAID 'OH YEAH DONT DO THAT' LIKE IT WAS NO BIG DEAL!! I'M LIVING ON A MIRACLE HERE PEOPLE!!!
Guys, I just want to say - this is SO important!! 🙌 I switched from azathioprine to mycophenolate last year and my GI issues dropped from 6x/day to 1x! I was crying in the bathroom every morning 😭 Now I take EC-MPS with a tiny bit of almond butter (doc approved!) and I feel like a new person!! If you're struggling, don't give up - there's a version out there that works for YOU!! 💪
Why are you all still talking about dosing and absorption? No one's talking about the real elephant in the room - the gut microbiome. Mycophenolate wrecks your microbiota, which is why you get diarrhea. Azathioprine? It’s just a slower poison. You think TPMT testing helps? It just gives you a false sense of security. The real fix is probiotics, fasting, and avoiding all processed food. I’ve been off both drugs for 2 years now - no rejection, no cancer, no diarrhea. Just raw kale and willpower.
I just want to say thank you for writing this. I’ve been on mycophenolate for 8 years and the diarrhea was crushing me. I thought I was the only one. Hearing about EC-MPS gave me hope. My sister just got a kidney transplant and I’m going to print this out for her doctor. You’re not just sharing facts - you’re saving lives.
So let me get this straight: you're telling me I need to wait 2 hours after eating to take my $600 pill... and then wait another 2 hours before my calcium supplement? And if I forget? I reject my new kidney? 😌 I guess I'll just start carrying a stopwatch and a lunchbox labeled 'Immunosuppressant Protocol Zone'.
Every human being deserves access to life-saving medicine. The fact that cost determines whether someone lives or dies is not a medical issue - it is a moral failure. Azathioprine may be cheaper, but it is not less valuable. We must demand equitable access, not just better dosing schedules. Compassion must guide policy, not profit margins.
You people are naive. TPMT testing is useless without pharmacogenomic interpretation. Most clinics don't even know how to read the results. You think the FDA cares? They approved the damn calculator because it looks like innovation. Meanwhile, your skin cancer is growing and you're too busy checking your MPA levels to notice.
Just returned from a transplant clinic in Perth - they're now using AI-driven MPA forecasting models combined with real-time gut pH monitoring. It’s wild. They adjust mycophenolate doses dynamically based on your diet, sleep, and even weather. No more guessing. No more 2-hour fasting rituals. The future is here - and it’s not in your pill bottle. It’s in the data.
Stop romanticizing this. Azathioprine is a relic. Mycophenolate is the gold standard. Anyone who still uses azathioprine in a high-resource setting is either lazy, cheap, or incompetent. And if you're in rural India? That’s tragic - but it doesn’t make azathioprine ‘still useful.’ It makes the healthcare system broken. Stop pretending poverty is a valid medical variable.
I’m the author of this post. Thank you all for engaging so thoughtfully. I’ve seen patients lose limbs from skin cancer because they didn’t know about the UV risk. I’ve seen people skip doses because they couldn’t afford the pill. This isn’t just science - it’s survival. Keep asking questions. Keep demanding tests. And if your doctor brushes you off? Find another one. Your life is worth more than a 10-minute appointment.