When your insurance plan suddenly stops covering your medication, it’s not just a paperwork issue-it’s a health crisis. Imagine taking Humira for Crohn’s disease for seven years, then waking up one day to find your monthly cost jumped from $50 to $650 because your plan moved it to a non-preferred tier. This isn’t rare. In 2024, 34% of Medicare beneficiaries experienced unexpected changes to their drug coverage, and 57% of patients got less than a month’s notice. Formulary changes don’t just affect your wallet-they can derail your treatment, increase ER visits, and even shorten your life.
What Is a Formulary, Really?
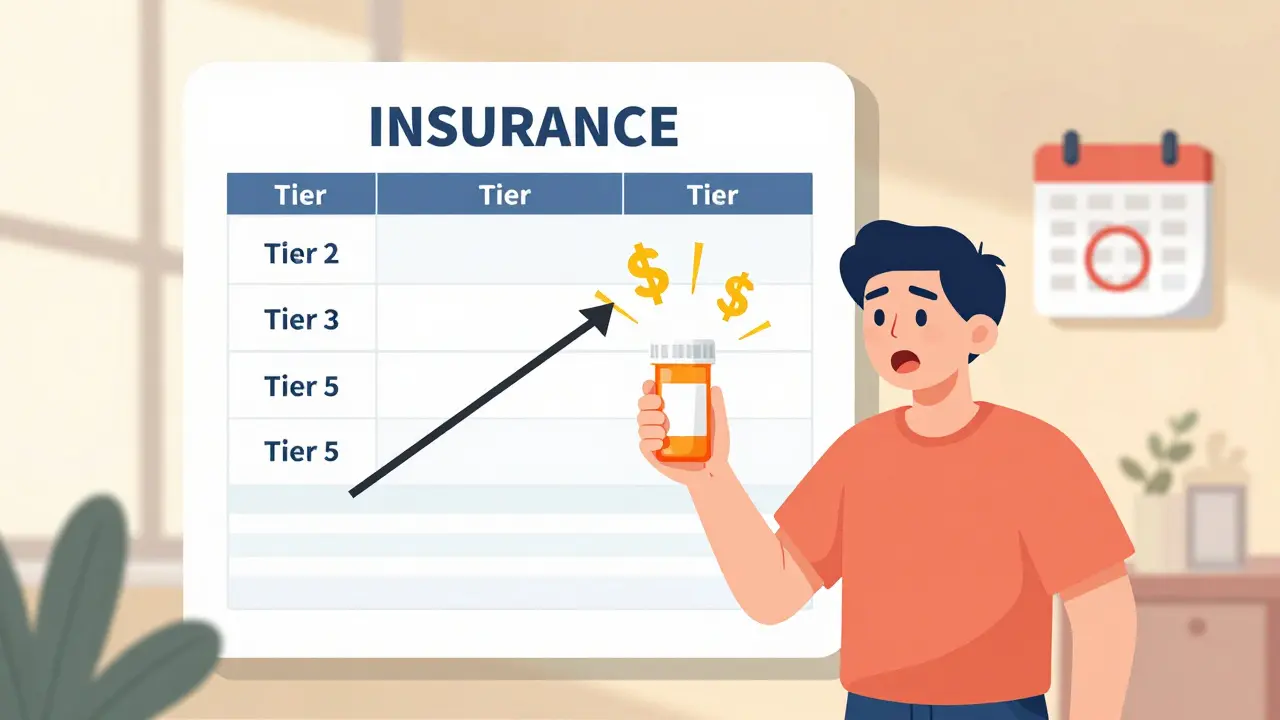
A formulary is your insurance plan’s list of covered prescription drugs. It’s not just a catalog-it’s a gatekeeper. Most plans use a tiered system: Tier 1 has low-cost generics, Tier 2 has preferred brand-name drugs, and Tier 3 or 4 includes expensive specialty medications. The higher the tier, the more you pay out of pocket. Some plans go even further: Tier 5 can demand 33% coinsurance on drugs like insulin or biologics.Formularies aren’t random. They’re shaped by pharmacy and therapeutics (P&T) committees that review clinical data, negotiate rebates with drugmakers, and weigh cost against effectiveness. Medicare Part D plans must cover at least two drugs per therapeutic class and update formularies within 120 days of a new drug’s FDA approval. Commercial plans often review theirs quarterly. And here’s the kicker: 92% of Medicare Part D plans and 87% of commercial plans use tiered formularies. That means almost every insured American is affected by these decisions.
Why Do Formularies Change?
Formularies change for three main reasons: cost, competition, and clinical evidence.First, drug prices spike. A new biologic enters the market, and the old one loses its rebate. The insurer drops the old drug from preferred status to push patients toward the cheaper option-even if it’s less effective. Second, generics become available. When a brand-name drug loses patent protection, insurers rush to move patients to the generic version. Third, new clinical data emerges. If a study shows a drug has dangerous side effects or doesn’t work as well as thought, it gets downgraded or removed.
But here’s what insurers don’t always tell you: changes aren’t always about health. Sometimes, it’s about profit. A 2023 study found that when a drug moved from Tier 2 to Tier 3, abandonment rates jumped 47%. For diabetes meds, it was 58%. That’s not just inconvenience-it’s patients skipping doses, skipping refills, or stopping entirely. And that leads to hospitalizations, complications, and higher long-term costs.
How Formulary Changes Hit Different Groups
Not everyone feels formulary changes the same way.Medicare beneficiaries get at least 30 days’ notice-sometimes 60-for non-urgent changes. That’s a lifeline. Commercial plan members? On average, they get 22 days. No warning. No grace period. Just a letter in the mail or a note in your online portal.
Low-income patients suffer the most. A Harvard study found that when formularies restrict access to essential drugs, emergency room visits among low-income Medicare enrollees rise by 12%. Why? Because they can’t afford the new copay. They wait too long. Their condition worsens. They end up in the ER.
Meanwhile, patients with rare diseases face near-total barriers. 73% of specialty drugs for conditions like MS or cystic fibrosis require prior authorization. That means your doctor has to fill out paperwork, wait for approval, and hope the insurer agrees your case is urgent enough. One patient spent three weeks fighting for temporary coverage after her Humira was dropped. She wasn’t alone.
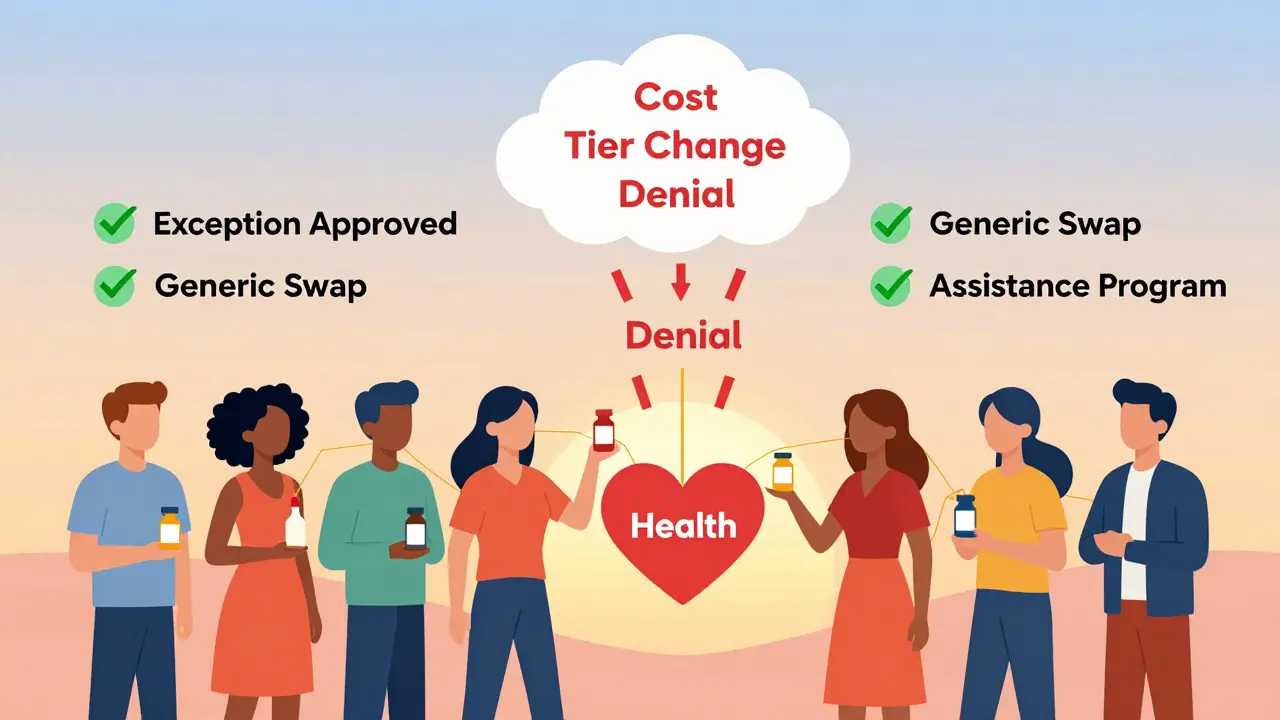
What You Can Do When Your Drug Is Removed
You’re not powerless. Here’s how to fight back.- Check your formulary before open enrollment. Every fall, insurers release their next year’s formularies. Use tools like Medicare’s Plan Finder or your insurer’s online formulary lookup. Search for every drug you take. Don’t assume it’s still covered.
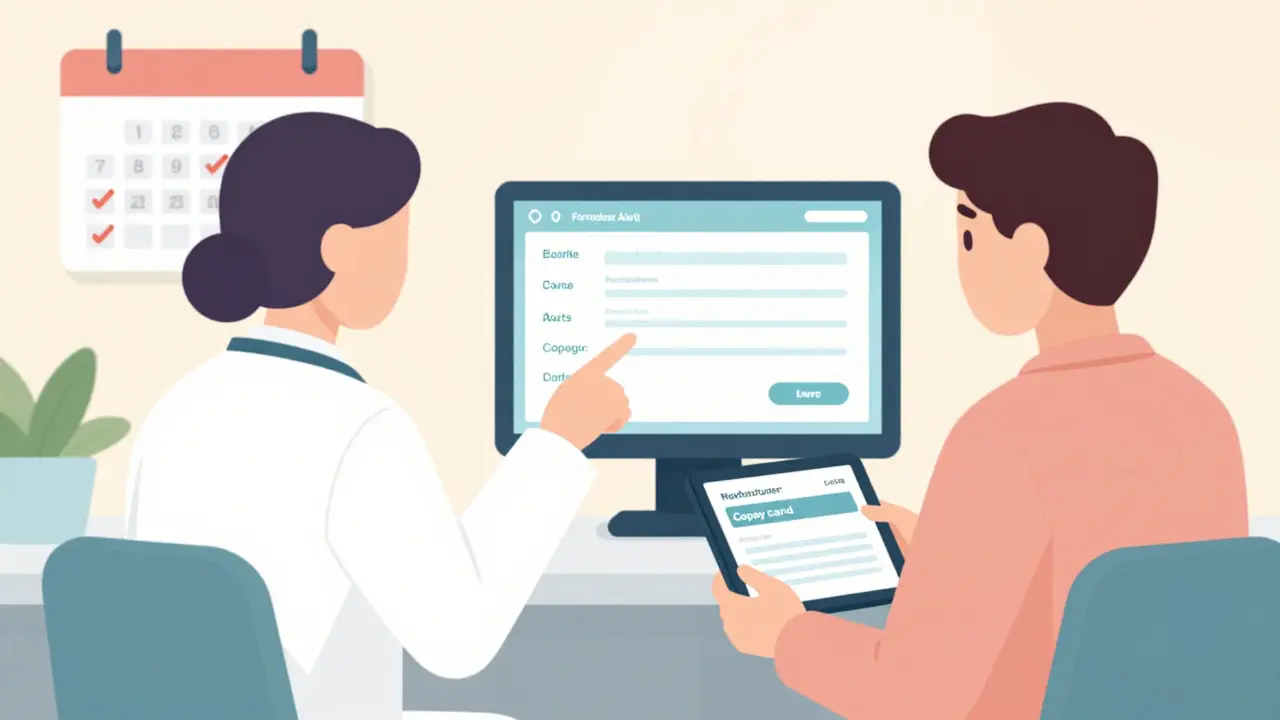
- Ask for a formulary exception. If your drug is removed or moved to a higher tier, you can request an exception. You need your doctor to write a letter explaining why the alternative won’t work for you. According to CMS, 64% of medically justified exceptions are approved.
- Use manufacturer assistance programs. Most big drugmakers offer copay cards, patient assistance programs, or free samples. In 2024, these programs covered $6.2 billion in patient costs. Check the drug’s official website or call the manufacturer directly.
- Switch to a therapeutic alternative. Your doctor might have a similar drug on a lower tier. For example, if your brand-name statin is dropped, there are five generic alternatives that work just as well. Don’t panic-ask your pharmacist or doctor for options.
- Appeal if denied. If your exception request is denied, you have the right to appeal. Medicare beneficiaries can call their State Health Insurance Assistance Program (SHIP). These free counselors helped 37% more people win appeals in 2023.
How Providers Can Prevent Disruptions
Doctors and clinics aren’t just bystanders-they’re frontline defenders.Large medical groups now use e-prescribing systems that check formulary status in real time. When a doctor writes a prescription, the system flags if the drug is off-formulary or requires prior auth. That means the patient gets an alternative before leaving the office. 76% of large practices use this tech.
Proactive clinics also monitor formulary updates 60 days in advance. They alert patients during routine visits. One nurse on AllNurses shared how her clinic did this: “We switched 12 patients to generic alternatives during their annual checkups. No one got caught off guard.” That’s the gold standard.
Don’t wait for the letter. If you’re managing chronic conditions like diabetes, hypertension, or rheumatoid arthritis, ask your provider: “What’s our plan if my drug gets pulled?” Make it part of your care routine.
The Bigger Picture: What’s Changing in 2025 and Beyond
Formularies are evolving-and fast.Starting in 2025, Medicare beneficiaries will pay no more than $2,000 a year out of pocket for drugs. That’s a game-changer. Insurers can’t keep pushing patients into expensive tiers if they’re capped. Expect to see fewer high-tier drugs and more flat-rate copays.
Value-based formularies are also rising. Instead of just cutting costs, some plans now pay based on outcomes. If a drug lowers hospitalizations or improves quality of life, the insurer pays more. These are used by 25% of large employers today-and that number is projected to hit 45% by 2027.
And then there’s AI. New tools can predict which patients are most likely to stop taking a drug if it moves tiers. One 2024 study showed these tools predict non-adherence with 89% accuracy. That means insurers will soon know exactly who will drop their meds-and maybe, just maybe, they’ll act before it happens.
What You Need to Remember
Formulary changes aren’t going away. But you don’t have to be a victim of them.Know your plan. Check your formulary every fall. Keep a list of your drugs and their tiers. Talk to your pharmacist. Ask your doctor about alternatives. Use manufacturer help. File exceptions. Appeal denials.
And if you’re a caregiver or advocate for someone with chronic illness-be their voice. Formularies are designed to save money. But they shouldn’t cost lives.
What happens if my insurance drops my medication?
If your insurance drops your medication, you can request a formulary exception through your plan. Your doctor must submit a letter explaining why the alternative won’t work for you. If denied, you can appeal. You also have 30-60 days to finish your current supply, depending on your plan. Meanwhile, check for manufacturer assistance programs or switch to a covered alternative.
How much notice do I get before a formulary change?
Medicare Part D plans must give you 30 to 60 days’ notice for non-urgent changes. Commercial plans are not required to give any minimum notice, but most provide around 22 days on average. Always check your plan’s website or member portal during open enrollment season-changes are often posted there first.
Can I switch plans if my drug is removed?
Yes, but only during specific enrollment periods. For Medicare, you can switch during the Annual Enrollment Period (October 15-December 7) or during a Special Enrollment Period if you qualify (like moving or losing other coverage). For commercial plans, you typically have to wait until your plan’s renewal date unless you experience a qualifying life event like job loss or divorce.
Are generic drugs always better than brand-name drugs?
For most medications, yes. Generics contain the same active ingredients and meet the same FDA standards as brand-name drugs. But for certain complex drugs-like biologics or those with narrow therapeutic windows-there can be differences in effectiveness or side effects. Always consult your doctor before switching, even if the insurer pushes you to a generic.
How do I find out if my drug is on my plan’s formulary?
Log in to your insurer’s website and use their formulary search tool. Medicare beneficiaries can use the Plan Finder tool at medicare.gov. You can also call your plan’s customer service or ask your pharmacist to check. Always verify coverage before filling a prescription, especially after major life changes or during open enrollment.
What is a formulary exception, and how do I get one?
A formulary exception is a request to cover a drug that’s not on your plan’s list or is restricted. To get one, your doctor must submit a letter explaining why the drug is medically necessary and why alternatives won’t work. You can submit this request online, by phone, or by mail. Approval rates are high-64%-when the request is supported by clinical evidence.
Do formulary changes affect my out-of-pocket costs?
Absolutely. Moving a drug to a higher tier can increase your copay by hundreds of dollars per month. For example, a drug that cost $50 a month on Tier 2 might jump to $650 on a specialty tier. That’s why checking your formulary before open enrollment is critical. Even small changes can add up to over $500 extra per year, according to a 2023 Health Affairs study.