Medication Drowsiness Risk Checker
Find Your Drowsiness Risk
Select your medication class to see drowsiness risk, half-life, and management strategies
Select a medication class above to see drowsiness risk information
Quick Reference Guide
| Medication Class | Incidence (%) | Half-Life (hrs) | Risk Level |
|---|---|---|---|
| Antihistamines | 50-70 | 4-12 | High |
| Tricyclic Antidepressants | 30-40 | 12-30 | Medium |
| Benzodiazepines | 40-60 | 2-30 | High |
| Beta-Blockers | 10-15 | 3-10 | Low |
| Opioids | 30-50 | 2-12 | High |
Medication‑induced drowsiness is a drug‑related condition where a person feels excessively sleepy or fatigued during the day because a medication depresses the central nervous system. Health authorities label it as drug‑induced somnolence (ICD‑10‑CM R40.0). Roughly 15‑20 % of adults report this side effect, and it can jeopardize driving, increase fall risk, and lower overall quality of life.
Key Takeaways
- Antihistamines, tricyclic antidepressants, benzodiazepines, beta‑blockers, and opioids are the top culprits.
- Switching the time of day you take a sleepy‑inducing drug can cut daytime fatigue by up to 70 %.
- Non‑sedating alternatives (e.g., second‑generation antihistamines) are now the market norm.
- Personalized testing and new wake‑promoting meds like solriamfetol are emerging options.
- Never stop a prescribed drug abruptly; discuss any changes with a health professional.
Why do some drugs make you sleepy?
The brain’s wake‑up system relies on neurotransmitters such as norepinephrine, dopamine, and histamine. When a medication blocks histamine receptors (first‑generation antihistamines) or enhances GABA activity (benzodiazepines, many opioids), the net effect is a slowdown of neuronal firing - the classic CNS‑depression pathway. A 2010 PubMed study (PMID 20656627) showed that receptor‑level inhibition correlates directly with subjective sleepiness scores.
Other mechanisms include:
- Reduced heart rate and blood pressure from beta‑blockers, which can lower overall energy. \n
- Indirect antihistamine effects from some tricyclic antidepressants that increase histamine turnover.
- Metabolic overload when opioids interact with other CNS depressants, raising the risk of respiratory depression.
Medication classes most associated with drowsiness
The following groups consistently top the adverse‑event charts. Each entry includes a brief description, typical drowsiness incidence, and a practical tip.
| Class | Common drugs | Incidence (%) | Typical half‑life (hrs) | First‑line management |
|---|---|---|---|---|
| Antihistamines | Diphenhydramine, Brompheniramine, Hydroxyzine, Meclizine | 50‑70 | 4‑12 | Switch to a second‑generation agent (loratadine, cetirizine) or take at bedtime. |
| Tricyclic antidepressants | Amitriptyline, Doxepin, Imipramine, Trimipramine | 30‑40 | 12‑30 | Gradual dose taper, consider newer SSRIs/SNRIs with lower sedative profiles. |
| Benzodiazepines | Alprazolam, Clonazepam, Diazepam, Lorazepam | 40‑60 | 2‑30 (depends on agent) | Limit to night‑time use, assess need for taper, avoid combining with opioids. |
| Beta‑blockers | Atenolol, Metoprolol, Propranolol | 10‑15 | 3‑10 | Check for cardio‑selective alternatives (nebivolol) or dose timing. |
| Opioids | Oxycodone, Hydrocodone, Morphine | 30‑50 | 2‑12 | Limit to lowest effective dose, separate from benzodiazepines, use non‑opioid analgesics when possible. |
Practical ways to tame medication‑induced sleepiness
Most patients see improvement by tweaking habits rather than changing the prescription outright.
- Adjust timing. Taking a sleepy drug at night instead of the morning can cut daytime fatigue by 50‑70 % (Harvard Health, 2023).
- Prioritize sleep hygiene. Aim for 8 + hours of consistent sleep, dim lights an hour before bedtime, and avoid screens after 9 p.m.
- Gentle exercise. A 20‑minute walk after lunch boosts circulation and offsets mild sedation.
- Hydration & nutrition. Dehydration worsens CNS depression; sip water regularly and keep protein handy.
- Limit alcohol and other depressants. Even a single glass of wine can double the drowsiness impact of a benzodiazepine.
- Consider caffeine strategically. A modest cup before a critical task can help, but avoid after noon to protect night‑time sleep.
For chronic cases, clinicians may prescribe wake‑promoting agents such as solriamfetol (Sunosi) off‑label, especially when other adjustments fail.
Special populations that need extra caution
Older adults are the most vulnerable. The American Geriatrics Society’s 2023 Beers Criteria flags >30 % of commonly prescribed senior meds as having drowsiness risk, contributing to 20‑30 % of falls. Start with the lowest dose, use non‑sedating alternatives, and involve a caregiver in monitoring.
Drivers and machine operators should treat any new daytime sleepiness as a safety red flag. The CDC recommends a minimum 8‑hour uninterrupted sleep window before operating a vehicle after taking a CNS depressant.
Pregnant or breastfeeding patients must discuss risks with a provider, as some antihistamines cross the placenta and can cause neonatal sedation.
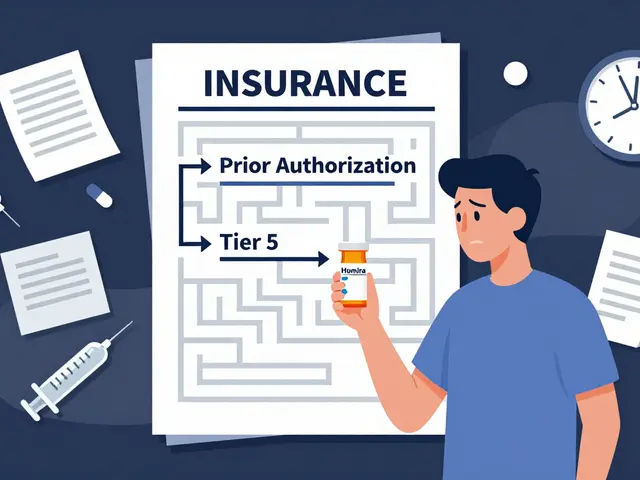
Emerging tools and future directions
Pharmaceutical firms are rolling out non‑sedating generations: second‑generation antihistamines now hold 78 % of the allergy market (IQVIA, 2023). Meanwhile, genetic panels like GeneSight can predict who is likely to feel sleepy on certain psychotropics, cutting adverse events by roughly 35 % (NeurologyAdvisor, 2023).
Digital medication‑management apps leveraging AI aim to flag high‑risk combos in real time; early pilots suggest a 25 % reduction in drowsiness‑related ER visits by 2027 (Digital Health Today, 2023). Still, the CDC stresses that direct patient counseling remains the most reliable preventive measure.
When to call your doctor
- Sleepiness persists despite timing changes or dose reduction.
- You experience unsteady gait, confusion, or breathing difficulty.
- You're unable to stay awake while driving or operating machinery.
- You're considering stopping a medication on your own.
Early professional input can prevent falls, accidents, and unnecessary medication switches.
Quick checklist for patients
- Identify the culprit drug (review package insert or ask pharmacist).
- Note when you take it and how it aligns with your daily routine.
- Apply at least two lifestyle tweaks from the list above.
- Document any change in sleepiness over a week.
- Share findings with your prescriber and discuss alternatives.
Frequently Asked Questions
Which over‑the‑counter meds cause the most drowsiness?
First‑generation antihistamines such as diphenhydramine (Benadryl) and hydroxyzine are the top OTC culprits, with up to 70 % of users reporting sleepiness.
Can I take caffeine to counteract drowsiness?
A modest cup can help for short‑term tasks, but regular afternoon caffeine can worsen nighttime sleep and may not solve the underlying drug effect.
Is it safe to stop a sedating antidepressant suddenly?
No. Abrupt cessation can trigger withdrawal, dizziness, and in rare cases serotonin syndrome. Taper under a clinician’s guidance.
What non‑drug options help reduce medication‑induced fatigue?
Improving sleep hygiene, regular light‑exercise, staying hydrated, and timing the dose for evenings are evidence‑based strategies that cut daytime sleepiness for many patients.
Are there any new prescriptions specifically for drug‑induced drowsiness?
Solriamfetol (Sunosi) is FDA‑approved for excessive sleepiness from narcolepsy or sleep apnea and is sometimes used off‑label for medication‑related fatigue under specialist supervision.




I switched my antihistamine to a non‑sedating formula and felt a big difference.
Switching the time you take a sleepy med can shave off half the drowsiness you feel during the day. The pharmacy data show that bedtime dosing of antihistamines drops daytime sleepiness by about 60 %. I’ve seen patients who moved their benzodiazepine to night‑only and suddenly regained focus at work. Just remember to talk to your prescriber before you shift anything around.
Ah, the classic ‘just move it to bedtime’ hack-so simple it feels like a meme. Yet the brain’s histamine trick still drags you down if the drug’s half‑life is absurdly long. You can’t outrun pharmacokinetics with a calendar shuffle forever. The real trick is picking a molecule that respects your waking hours. Until then, we’re all just bottle‑tipping the clock.
Adjusting the dose timing is often the first step before considering a switch. It’s a low‑risk maneuver that can be tried under pharmacist guidance.
While your suggestion sounds reasonable, let us not ignore the underlying metabolic interactions that persist regardless of the hour. A chronopharmacologic shift does not neutralize CYP450 inhibition, especially with tricyclics. Therefore, a thorough medication reconciliation remains indispensable.
Non‑sedating antihistamines like loratadine have become the default for many clinicians. They give you relief without the heavy eyelid‑drooping effect of older formulas.
When a patient reports feeling like a walking nap zone, the first thing I do is verify the exact medication schedule.
I ask for the time of day each dose is taken, the formulation, and whether any over‑the‑counter products are in the mix.
Next, I cross‑check the drug’s half‑life against the patient’s activity pattern to see if there is a mismatch.
If the drug has a long half‑life and the patient needs alertness in the morning, I look for a short‑acting alternative or a dose reduction.
For antihistamines, the move from diphenhydramine to cetirizine is a textbook example of a win‑win scenario.
I also evaluate any co‑prescribed CNS depressants, because the combination effect is often greater than the sum of its parts.
In cases where the patient cannot switch drugs, I counsel on strategic caffeine use-one cup before a critical task, not after noon.
Hydration is another cheap but effective tool; dehydration can amplify sedation by reducing cerebral perfusion.
Light exercise, such as a brisk 15‑minute walk after lunch, helps reset the circadian drive and can offset mild drowsiness.
When the medication is indispensable, such as a beta‑blocker for heart failure, I consider timing the dose for the evening and monitoring blood pressure trends.
I also keep an eye on the patient’s fall risk, especially in older adults, and may involve a physical therapist for balance training.
If lifestyle tweaks fail, I discuss wake‑promoting agents like solriamfetol with the prescribing specialist, remembering the off‑label nature of that approach.
Throughout the process I document changes in a simple checklist so the next provider can see what has been tried.
Patient education is key; they need to understand that stopping a drug abruptly can cause rebound symptoms or withdrawal.
Finally, I schedule a follow‑up in two weeks to reassess sedation levels and adjust the plan as needed.
I hear you-feeling drowsy can really throw a wrench into daily life. Small habits like a short walk and a glass of water often make a surprising difference. Keep a journal of when you feel the sleepiness hit, it helps the doctor fine‑tune the regimen.
All that checklist stuff sounds like bureaucratic busywork. Most people just need a stronger dose of coffee, not a whole protocol. If the med is making you drowsy, maybe it’s not the right med at all.
Pharmacokinetic alignment with circadian rhythms is a scientifically supported strategy. Adjustments should be documented to evaluate efficacy.
The fog descended fast, turning a simple morning into a blur of inertia. Only a swift medication review lifted that veil.
Timing changes are low risk and often effective. Always involve your prescriber.
Try a non‑sedating antihistamine. It can cut the sleepiness.
Utilizing second‑gen H1 antagonists (e.g., cetirizine) leverages peripheral H1 blockade while sparing central H1 receptors 🚀, thereby preserving wakefulness 🌞.
Remember, you’re not alone in navigating these side effects. Your healthcare team is there to help you find a balance.