More than 4 in 10 older adults in the U.S. are taking five or more prescription drugs daily. That’s not just common-it’s dangerous. Many of these medications were started years ago for conditions that no longer apply, or they’re now doing more harm than good. The truth is, deprescribing isn’t about cutting corners. It’s about cleaning up clutter that’s putting seniors at risk.
What Is Deprescribing, Really?
Deprescribing means stopping or lowering the dose of a medicine when the risks outweigh the benefits. It’s not quitting meds cold turkey. It’s not ignoring doctors. It’s a careful, planned process backed by science. The term was first used in 2003 by an Australian doctor who noticed how often older patients were drowning in pills they didn’t need. Today, it’s a recognized part of geriatric care.Think of it like this: if you started taking a pill for high blood pressure ten years ago and your pressure is now normal, why keep taking it? What if that same pill is now causing dizziness, falls, or kidney problems? That’s when deprescribing kicks in. The goal isn’t to reduce the number of pills for the sake of it. It’s to match treatment to what matters now-your health, your safety, your quality of life.
When Should You Consider Stopping a Medication?
There are clear signs that it’s time to talk to a doctor about deprescribing:- New symptoms show up after starting a drug. Did you start a new pill and then feel foggy, weak, or off-balance? That could be a side effect, not aging. Dizziness, confusion, nausea, or sudden fatigue are red flags.
- You’ve been diagnosed with advanced illness. If you have late-stage dementia, heart failure, or cancer that’s no longer treatable, some medications-like cholesterol drugs or diabetes pills-no longer make sense. They won’t extend your life, but they might make your days harder.
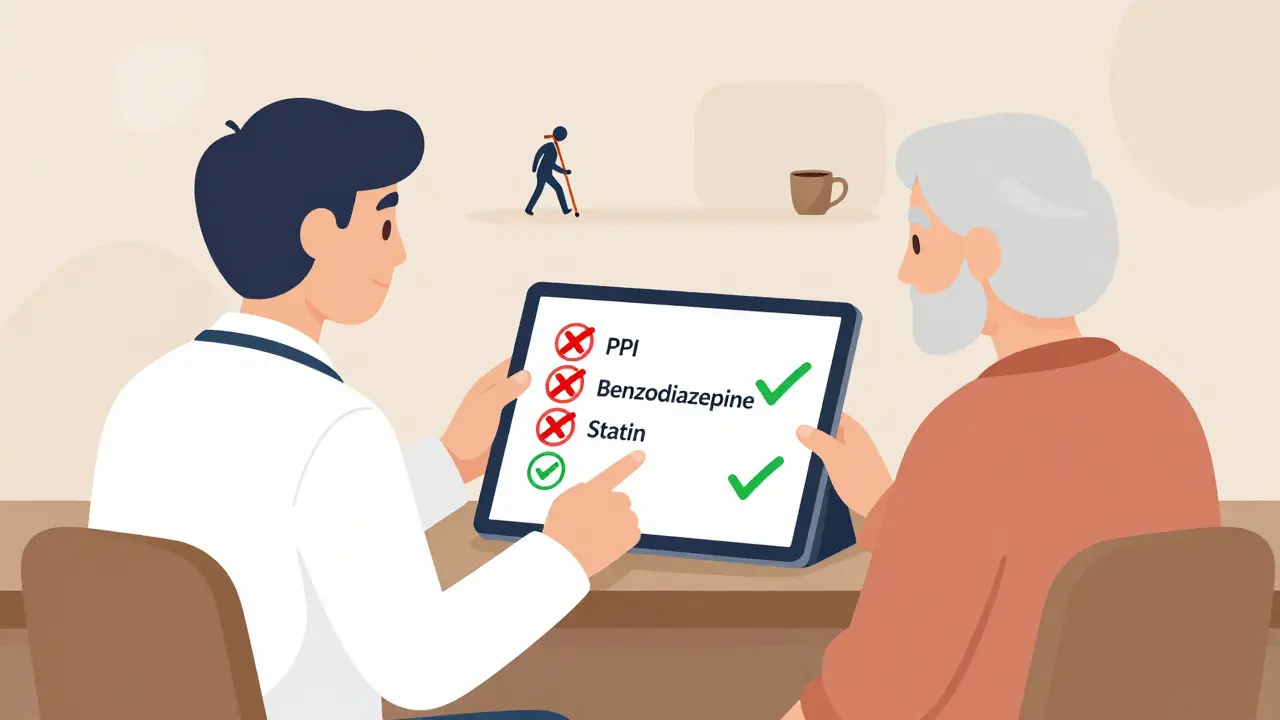
- You’re on high-risk drugs. Some medications are especially dangerous for older adults. Benzodiazepines (like Valium or Xanax) raise fall risk. Anticholinergics (found in some sleep aids and bladder meds) can cause memory loss. Long-term proton pump inhibitors (PPIs) for heartburn can weaken bones and cause infections. These are top candidates for review.
- You’re taking preventive meds with no short-term benefit. Statins for cholesterol, aspirin for heart protection, or vaccines like pneumonia shots? Great when you’re healthy. But if you’re 85, frail, and living at home, the long-term benefit of a statin might be years away-while the side effects are happening now.
The American Geriatrics Society and the American Academy of Family Physicians both say: Review every medication at every visit. Don’t assume a pill is still needed just because it’s been on your list for years.
How Do Doctors Decide What to Stop?
There’s no one-size-fits-all list. But experts use tools to guide decisions:- Beers Criteria - Updated regularly by the American Geriatrics Society, this list identifies drugs that are risky for seniors, like certain antihistamines, muscle relaxants, and sleep aids.
- STOPP Criteria - Focuses on inappropriate prescribing, like giving multiple drugs that do the same thing or combining meds that increase side effects.
- Pharmacist reviews - Clinical pharmacists are trained to spot drug interactions, duplicate therapies, and outdated prescriptions. Studies show they reduce inappropriate meds by up to 40% in older adults.
These tools aren’t rules-they’re starting points. A doctor will look at your overall health, how long you’ve lived with a condition, your life expectancy, and what matters most to you. If you want to stay active and independent, a drug that makes you sleepy or dizzy might not be worth keeping.
Why Is Polypharmacy So Common?
It’s not just about poor care. It’s systemic. Here’s how it happens:- Specialists don’t talk to each other. Your cardiologist prescribes a beta-blocker. Your rheumatologist adds a painkiller. Your primary care doctor doesn’t know both are happening. Each adds a med. No one steps back to see the whole picture.
- Refills become automatic. Most prescriptions are renewed without review. A pill gets refilled for years because no one ever said to stop.
- Doctors aren’t trained to stop. Medical schools teach how to prescribe. Few teach how to stop. A 2019 study found that 90% of guidelines explain how to start a drug-but only 1 in 5 explain how to stop it.
- Patient fear plays a role. Many seniors worry that stopping a drug will make their condition worse. They don’t know it’s safe to try.
Between 1994 and 2014, the percentage of U.S. seniors on five or more medications tripled. That’s not progress. That’s a public health problem.
What Happens When You Stop a Drug?
Some people think stopping meds will cause a rebound effect-like blood pressure shooting up or pain returning. Sometimes it does. That’s why deprescribing is done slowly, one drug at a time.For example:
- Stopping a PPI (like omeprazole) might cause temporary heartburn-but that usually fades in 2-4 weeks. Many people find they don’t need it anymore.
- Reducing a sleep aid like zolpidem can lead to insomnia at first, but most seniors adjust within a month and sleep better without the drug.
- Stopping a statin in a frail 80-year-old doesn’t increase heart attack risk-it just removes dizziness, muscle pain, and liver stress.
Studies show that when deprescribing is done right, adverse drug events drop by 17-30%. Hospital readmissions fall by 12-25%. And seniors report feeling clearer-headed, stronger, and more in control.
How to Start the Conversation
You don’t need to wait for a crisis. Here’s how to bring it up:- Make a list of every pill, supplement, and over-the-counter drug you take-including doses and why you take them.
- Ask: “Which of these are still helping me? Which might be causing problems?”
- Request a full medication review during your next visit. Say: “I’d like to go over my list and see what we can safely stop.”
- Ask if a pharmacist can help. Many clinics now offer free medication reviews.
- Don’t stop anything on your own. Work with your doctor to taper safely.
Bring a family member. Write down answers. If the doctor says “it’s fine,” ask: “What would happen if I stopped this?” If they don’t know, that’s a sign it’s time to get a second opinion.
What About Chronic Conditions?
You might be thinking: “But I have diabetes. What if I stop my meds?”Good question. Deprescribing doesn’t mean abandoning treatment. It means tailoring it. For example:
- If your A1C is stable at 7.2% and you’re 82, your doctor might switch from insulin to a less risky oral drug-or even stop it entirely if your risk of low blood sugar outweighs the benefit.
- If you have mild hypertension and no history of stroke, your target blood pressure might change from 120/80 to 140/90. That could mean dropping one pill.
Life expectancy matters. If you’re 90 with limited mobility and no desire for aggressive treatment, the goal shifts from preventing a heart attack in 10 years to feeling well today.

What’s Changing in 2026?
Technology is catching up. Electronic health records now have built-in alerts for risky drug combinations. Apps like Deprescribing.org offer free, evidence-based guides for stopping PPIs, benzodiazepines, and antipsychotics-with printable checklists and videos.Some clinics now assign a “medication coach”-often a pharmacist-who follows up after a deprescribing attempt. They call you two weeks later to see how you’re feeling. That kind of support makes a huge difference.
The World Health Organization now lists deprescribing as a global patient safety priority. Medicare is starting to track how often seniors have medication reviews. That means more doctors will be encouraged-and eventually required-to do them.
What’s the Biggest Mistake People Make?
Thinking deprescribing means giving up. It doesn’t. It means choosing better care. It means saying: “I don’t want to live on a pile of pills that make me feel worse.”One woman, 86, was on eight medications. She felt tired all the time and had fallen twice. After a pharmacist review, three drugs were stopped: a sleep aid, a stomach acid reducer, and a cholesterol pill. Within a month, she was sleeping better, walking without a cane, and eating meals with her grandchildren again.
That’s not a miracle. That’s smart medicine.
Final Thought: Your Meds Are Not Permanent
Every prescription is a trial. Every refill is a chance to ask: “Is this still helping?”Seniors aren’t just patients. They’re people who want to live well, not just live longer. The best care isn’t about adding more drugs. It’s about removing the ones that don’t belong.
Is it safe to stop taking medications on my own?
No. Stopping some medications suddenly can be dangerous. Blood pressure pills, antidepressants, seizure meds, and steroids need to be tapered slowly under medical supervision. Always talk to your doctor before making changes.
What if my doctor says I need all my meds?
Ask why. Request a review using the Beers Criteria or STOPP guidelines. Ask if a clinical pharmacist can help. If your doctor dismisses your concerns, consider seeing a geriatrician or a primary care provider who specializes in older adults. Your health is your priority.
How long does it take to see results after stopping a medication?
It varies. Some side effects, like dizziness or confusion, improve in days. Others, like muscle pain from statins, may take weeks. Withdrawal symptoms from sleep aids or antidepressants can last up to a month. Patience and monitoring are key. Keep a symptom journal to track changes.
Can deprescribing help with memory problems?
Yes. Many common medications-like antihistamines, bladder pills, and sleep aids-have anticholinergic effects that can fog your thinking. Studies show that removing these drugs can improve memory and attention in older adults, even those with early dementia.
Are over-the-counter drugs included in deprescribing?
Absolutely. Many seniors take OTC meds daily-like antacids, sleep aids, or pain relievers-that interact with prescriptions or cause side effects. A full medication review includes everything you take, even if you bought it without a prescription.
Will stopping meds make my conditions worse?
Not if done correctly. Deprescribing targets drugs with little benefit and high risk. For example, stopping a statin in a frail 85-year-old doesn’t increase heart attack risk-it removes side effects. Studies show disease outcomes stay stable or improve when inappropriate meds are removed.
Where can I find help with deprescribing?
Start with your primary care doctor or pharmacist. Many community pharmacies offer free medication reviews. You can also visit Deprescribing.org for free, evidence-based guides. Ask for a referral to a geriatrician or a clinical pharmacist who specializes in older adults.





I’ve seen this happen with my mom-eight meds, zero energy, constantly dizzy. We talked to her pharmacist and cut three. She started cooking again. No magic, just common sense.
So we’re telling seniors to stop meds… but not to question why they were prescribed in the first place? 😏
My aunt stopped her statin last year-no heart attack, no drama. Just less brain fog and way more walks with the grandkids. 🙌
Let’s be brutally honest here-the entire medical-industrial complex is built on perpetual prescribing. Pharma spends billions convincing doctors that every minor fluctuation needs a pill, and then they train doctors to never question it. Medical schools don’t teach deprescribing because it’s not profitable. The system is designed to keep you medicated, not healthy. You think your doctor’s giving you advice? They’re following protocols written by people who profit when you stay sick. Deprescribing isn’t just smart-it’s an act of rebellion against a broken system that sees you as a walking prescription pad.
America’s problem isn’t too many pills-it’s too many people who think they know better than their doctors. If you’re gonna stop meds, at least have the decency to be under care. Not just some guy on Reddit telling you to quit your blood pressure drug.
My dad’s on five meds. We asked his GP to review them last month. Two got cut. He says he feels like he’s 65 again. Simple stuff, really.
You got this. Talking to your doctor about meds is the bravest thing you can do for your future self.
OMG YES!! My grandma stopped her anticholinergic sleep aid and suddenly remembered my birthday 🥹❤️
Deprescribing isn’t just a medical concept-it’s a moral one. We treat aging like a disease to be managed with pills, rather than a life stage to be lived with dignity. When we stop asking, ‘What can we add?’ and start asking, ‘What can we remove?’-that’s when real care begins. The Beers Criteria and STOPP aren’t just lists; they’re ethical guidelines for not harming people who’ve already lived long enough. We owe our elders more than a pharmacy receipt. We owe them clarity, safety, and the freedom to feel human again.
THIS IS A GOVERNMENT PLOT TO CONTROL THE ELDERLY!!! They want you dependent on pills so they can track you through your prescriptions!! I heard they’re putting microchips in the fill bottles!! And the pharmacists? They’re all undercover agents!! You think your doctor cares? They’re paid by Big Pharma to keep you on the wheel!! STOP TAKING EVERYTHING!! GO NATURAL!! CAYENNE PEPPER AND APPLE CIDER VINEGAR WILL SAVE YOU!!!
And yet, Kanchan, the data doesn’t lie: a 2022 JAMA study showed that when seniors stopped anticholinergics, cognitive scores improved by 18% in six months. No microchips needed. Just science.
Every pill is a story. Some are chapters of survival. Others are footnotes from a life that no longer exists. We cling to them like relics. But time doesn’t ask for permission to change your needs. The real question isn’t whether you can stop the drug-it’s whether you can forgive yourself for needing it in the first place.
People like you think this is ‘smart medicine.’ It’s just lazy medicine. If you’re too tired to manage your health, maybe you shouldn’t be living alone. Stop blaming the pills and start blaming the lack of discipline.