SSRI + NSAID GI Bleeding Risk Calculator
This tool estimates your risk of upper gastrointestinal bleeding when taking both an SSRI and an NSAID. Based on factors like age, medical history, and medication usage.
Important: This is a simplified risk assessment tool for educational purposes only. Always consult with your healthcare provider for personalized medical advice.
When you take an antidepressant and a pain reliever at the same time, the combo can turn a routine prescription into a serious stomach bleed. The link between SSRIs and selective serotonin reuptake inhibitors used for depression, anxiety and several other conditions and NSAIDs non‑steroidal anti‑inflammatory drugs such as ibuprofen, naproxen or diclofenac is one of the most under‑appreciated drug interactions in primary care. Below you’ll find a step‑by‑step guide that walks you through why the risk spikes, who should worry most, and exactly what you can do to stay safe.
Why the combination matters
About one in eight adults in the United States fills a prescription for an SSRI, and roughly the same proportion uses NSAIDs on a regular basis. That overlap means millions of people could be walking a tightrope between mental‑health relief and a potentially life‑threatening bleed. A 2022 meta‑analysis in Nature Scientific Reports showed a 75% higher odds of upper gastrointestinal bleeding bleeding that occurs in the stomach or duodenum, often presenting as black tarry stools or vomiting blood when the two drug classes are taken together versus NSAID use alone.
How the drugs collide inside your body
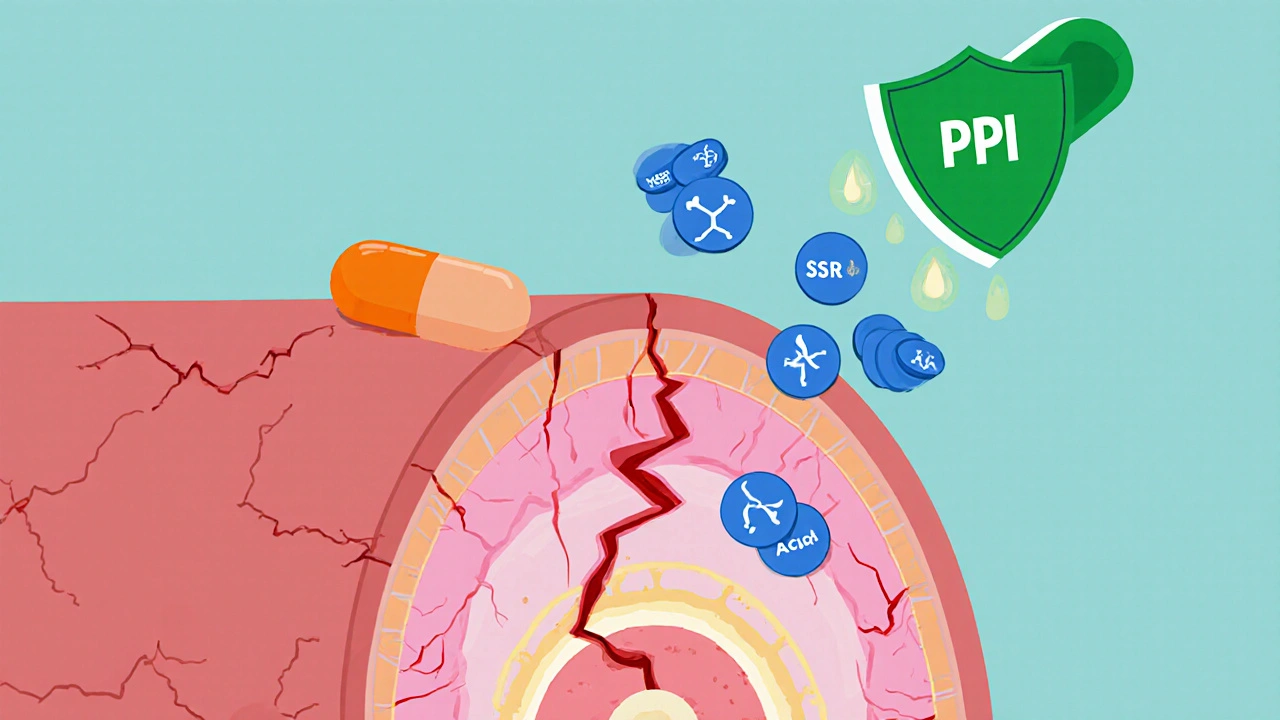
SSRIs block the serotonin transporter on platelets. Platelets need serotonin to clump together and form the first plug that stops bleeding. When serotonin uptake is hampered, clot formation weakens.
NSAIDs, on the other hand, scrape the stomach lining and shut down cyclooxygenase enzymes that produce protective prostaglandins. Without prostaglandins, the gastric mucosa becomes fragile and more prone to erosion.
The double hit-impaired platelet plug plus a compromised lining-creates a perfect storm for bleeding. The effect isn’t merely additive; studies show the interaction behaves multiplicatively, pushing the odds even higher than you’d expect from the sum of the parts.
Who’s at the highest risk?
- Adults over 65 years old - age alone reduces platelet function.
- Anyone with a history of peptic ulcer disease or prior GI bleed.
- Patients already on low‑dose aspirin or anticoagulants (warfarin, DOACs).
- Heavy NSAID users (>1,200 mg ibuprofen‑equivalent per day) or those on high‑dose SSRIs for more than three months.
Even younger, healthy adults can bleed when the dosage or duration climbs, but the numbers climb steeply in the groups above.
How big is the risk? Numbers that matter
A 2002 JAMA Internal Medicine study found the combination produced more than a 12‑fold increase in upper GI bleed compared with non‑users. In absolute terms, the baseline annual bleed rate for NSAID‑only users hovers around 0.5 %. Adding an SSRI pushes that to roughly 1.5 %-a three‑point jump that translates to thousands of hospitalizations each year.
When you throw low‑dose aspirin into the mix, the odds skyrocket again, matching the bleeding risk seen with full anticoagulation in high‑risk patients.
Below is a snapshot of odds ratios from major studies:
| Drug combo | Odds Ratio (OR) | Reference |
|---|---|---|
| NSAID alone | 2.0-4.0 | JAMA 2002 |
| SSRI alone | 1.5-2.0 | Digestive Diseases 2023 |
| SSRI + NSAID | 1.75 (vs NSAID alone) | Nature Sci Rep 2022 |
| SSRI + NSAID + Aspirin | >12.0 | JAMA 2002 |
Prevention strategies that actually work
The American Gastroenterological Association’s 2020 guideline recommends proton pump inhibitor (PPI) co‑therapy for anyone who must stay on both drug classes. A 2017 Lancet analysis showed PPIs cut the absolute bleed risk from about 1.5 % to 0.5 % per year-a 70 % relative reduction.
Key steps for clinicians and patients:
- Assess risk first. Use the AIMS65 score or the newer GI‑BLEED calculator (integrated in many EHRs) to quantify individual risk.
- If risk is moderate‑to‑high, start a PPI such as omeprazole 20 mg daily (or pantoprazole 40 mg) alongside the NSAID.
- Whenever possible, replace a non‑selective NSAID with a COX‑2‑selective agent like celecoxib a COX‑2 selective NSAID that carries a lower GI bleed risk. The same 2022 meta‑analysis gave celecoxib an OR close to 1.16, essentially neutral.
- For chronic pain, switch to acetaminophen paracetamol, a pain reliever that does not irritate the stomach nor interact with platelets. The Haghbin 2023 review found no increased bleed signal.
- Limit NSAID dose and duration. Aim for the lowest effective ibuprofen‑equivalent dose (<1,200 mg/day) and reassess after 30 days.
- Educate patients. A simple handout that lists “SSRI + ibuprofen = bleed risk” can cut inappropriate prescribing by two‑thirds, according to a 2021 JAMA quality‑improvement trial.
For patients already on low‑dose aspirin, the safest route is usually to pause the aspirin (if cardiovascular risk allows) and start a PPI. If aspirin can’t be stopped, the combination of PPI + COX‑2 inhibitor + SSRI is the most protective regimen.
Choosing safer pain relievers for antidepressant users
Here’s a quick comparison of common analgesics when paired with SSRIs:
| Medication | GI bleed risk with SSRI | Typical dose |
|---|---|---|
| Ibuprofen | Moderate‑high (OR ~1.8) | 200-400 mg q6‑8h |
| Naproxen | Higher (OR ~2.1) | 250-500 mg bid |
| Celecoxib | Low (OR ~1.2) | 100-200 mg daily |
| Acetaminophen | None detected | 500-1000 mg q6h |
When the analgesic choice is not obvious, start with acetaminophen for mild‑to‑moderate pain, reserve celecoxib for cases where inflammation is a key driver, and keep ibuprofen or naproxen as a last resort-always with a PPI cover.
Putting the plan into practice - a clinical workflow
Many electronic health records now include built‑in alerts for the SSRI‑NSAID combo. A 2020 BMJ Quality & Safety study showed those alerts shaved 32 % off bleed events. Here’s a simple three‑step workflow you can adopt, even without fancy EHR support:
- Screen every new prescription: ask the patient if they’re already on an SSRI or an NSAID.
- Risk‑stratify using the GI‑BLEED calculator (or a quick AIMS65 check). Flag anyone over 65, with prior ulcer, or on aspirin.
- Act:
- Prescribe a PPI if the combo can’t be avoided.
- Switch NSAID to celecoxib or acetaminophen when feasible.
- Document the interaction in the medication list with a note: “SSRI + NSAID - PPI started.”
Follow‑up within 30 days to reassess pain control and gastrointestinal symptoms. Adjust therapy based on response.

What’s on the horizon?
Recent advances promise even finer‑tuned prevention:
- GI‑BLEED risk calculator - now embedded in most major EHR platforms, it adds variables like CYP2C19 genotype, giving a personalized percentage risk.
- Pharmacogenomics - poor metabolizers of CYP2C19 have higher plasma SSRI levels, which may boost the platelet effect. Testing could steer clinicians toward drugs like vortioxetine, which showed 40 % fewer bleeds in a 2022 trial.
- New analgesic formulations - researchers are experimenting with gastro‑coated NSAID tablets that release the drug beyond the stomach, potentially eliminating mucosal injury.
- Regulatory moves - the FDA’s Sentinel Initiative will soon release a massive real‑world safety dataset on all SSRI‑NSAID combos, helping refine guidelines further.
Until those tools become routine, the proven trio of risk assessment, PPI protection, and smarter analgesic choice remains the best defense.
Quick checklist for patients and providers
- Identify if the patient is on an SSRI and an NSAID.
- Determine age, ulcer history, aspirin or anticoagulant use.
- Start a PPI if the combination can’t be stopped.
- Consider switching to celecoxib or acetaminophen.
- Use the GI‑BLEED calculator for a numeric risk estimate.
- Schedule a follow‑up visit within a month.
Frequently Asked Questions
Can I take any NSAID with my SSRI?
Non‑selective NSAIDs (ibuprofen, naproxen, diclofenac) increase bleed risk substantially. If you must use an NSAID, a COX‑2 selective agent like celecoxib plus a PPI is the safest route.
Do over‑the‑counter antacids protect against bleeding?
Antacids neutralize stomach acid temporarily but don’t prevent mucosal injury or platelet dysfunction. Only a PPI or an H2 blocker (like famotidine) provides lasting protection.
Is acetaminophen completely safe with SSRIs?
Current evidence shows no interaction that raises GI bleed risk. It’s the go‑to analgesic when you’re on an SSRI, unless the patient has liver disease that limits acetaminophen dosing.
How long should I stay on a PPI?
If the SSRI‑NSAID combo is indefinite, continue the PPI long‑term (usually 20-40 mg daily). If you can taper off the NSAID, reassess after 2-3 months and consider stopping the PPI if ulcer risk is low.
What warning should my pharmacy label include?
A clear statement such as “Do not take NSAIDs (ibuprofen, naproxen, etc.) without a doctor’s advice while using this antidepressant - risk of serious stomach bleeding.”
Keeping these points in mind can turn a potentially dangerous prescription into a well‑managed treatment plan. The key is awareness, risk assessment, and a proactive preventive strategy.





Pharma and the govt are colluding to keep you on risky drug combos!
The risk is real and you shouldn't ignore it. Simple math says a 1.5% bleed rate means many hospital visits. Stay aware and talk to your doctor. Don't think a couple of pills are harmless. Protect yourself.
Let me break it down for anyone still clueless about the SSRI‑NSAID disaster.
The combination is not a harmless coincidence, it is a textbook case of pharmacology gone rogue.
SSRIs sabotage platelet serotonin, leaving your blood without the first line of defense.
NSAIDs then strip the stomach lining, removing the protective barrier that keeps the acid at bay.
When both hit together, the result is a perfect storm that can bleed you out faster than a bad movie plot twist.
Studies have shown a 75% increase in odds, but the real‑world numbers are even more brutal.
Imagine a million patients, and you end up with tens of thousands of emergency visits each year.
That is not a statistic to shrug off; it is a public health crisis screaming for action.
Doctors should be prescribing PPIs as a default co‑therapy, not an after‑thought.
Patients need to know that over‑the‑counter ibuprofen with their antidepressant isn’t a free pass.
Switching to COX‑2 inhibitors or acetaminophen can cut the risk dramatically, as the data clearly indicate.
And for anyone on aspirin, the risk multiplies again, reaching the level of full anticoagulation.
The bottom line is simple: you cannot treat pain and depression in isolation without considering the gut.
If you’re not listening to your doctor’s advice on PPIs, you’re gambling with your life.
So, before you pop another tablet, think about the hidden price you might be paying.
The interplay of serotonin and prostaglandins, as we dissect, is not merely a biochemical footnote, but a profound lesson in systemic vulnerability, an echo of the body's fragile equilibrium, demanding our utmost respect, and a reminder that medicine is an art as much as a science.
One must consider the cascade of effects, the cascade of consequences, the cascade of patient outcomes, before prescribing.
This is a classic case of risk amplification that many overlook.
From a data perspective the odds are undeniable.
Clinicians should incorporate risk calculators into routine visits.
Patients benefit from clear guidance on PPI co‑therapy.
Hey folks 😊, just a heads‑up that mixing those meds can be a real nightmare 😬. If you’re on both, consider a PPI and maybe switch to acetaminophen 🩺.
Dear readers, it is advisable to evaluate the pharmacological synergy and adopt gastroprotective measures accordingly.
Yo, this combo is like a bad mixtape lol.
U gotta watch out, especially if u got a history of ulcers.
Switching to 2b safe meds can save u a lot of hassle.
Everyone, please take a moment to consider your medication list! 🌟
Adding a PPI is a simple step that can protect your gut. 💊💙
Think of the gut as a bridge; if two forces erode it simultaneously, collapse is inevitable.
One must not disregard the empirical evidence suggesting a synergistic hemorrhagic propensity when serotonergic reuptake inhibitors co‑administered with cyclooxygenase antagonists are employed in clinical practice.
The philosophical implication is stark: we cannot separate mental health treatment from physical wellbeing without courting disaster.
Ignorance is a luxury no patient can afford.
Let’s keep the conversation constructive and focus on actionable steps-use PPIs, consider COX‑2 agents, and stay educated.