Oral Thrush Risk Assessment
How to assess your risk
Answer these questions to see your risk level for developing oral thrush from inhaled corticosteroids.
Your Risk Assessment
Using an inhaled corticosteroid (ICS) inhaler every day can keep your asthma under control-but it can also leave you with a white, patchy tongue, a sore throat, or a voice that sounds like you’ve been shouting for hours. These aren’t rare side effects. They’re common, preventable, and often ignored. If you’ve been told to rinse your mouth after using your inhaler but never really did, you’re not alone. But here’s the truth: skipping that simple step can turn a minor annoyance into a recurring infection or chronic hoarseness that lasts weeks.
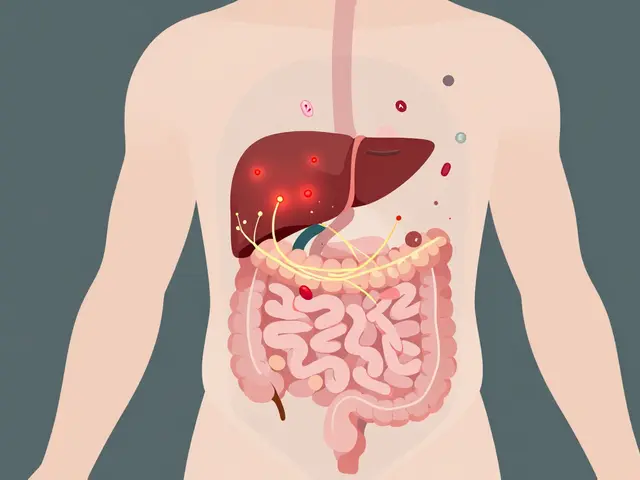
Why Your Inhaler Causes Oral Thrush
Inhaled corticosteroids like fluticasone (Flovent), budesonide (Pulmicort), and beclomethasone (Qvar) are designed to reduce inflammation in your lungs. But when you breathe in the medication, a portion of it doesn’t make it to your lungs. Instead, it sticks to the back of your throat and your tongue. That’s where the problem starts.Corticosteroids suppress local immune responses. In your mouth, that means the tiny fungi-mostly Candida albicans-that normally live harmlessly in your saliva can start multiplying unchecked. What begins as a slight white film can turn into thick, cottage cheese-like patches on your tongue, inner cheeks, or even your tonsils. These patches can be painful, make swallowing hard, and cause a burning sensation or loss of taste. In severe cases, the tissue underneath bleeds if you scrape it off.
It’s not just about how strong your inhaler is. It’s about how you use it. People using high doses-above 800 mcg per day of beclomethasone equivalent-are at higher risk. So are older adults, people with diabetes (especially if HbA1c is over 7.0%), and those with dry mouth or poor dental hygiene. Even a single missed rinse after your nightly inhaler can be enough to tip the balance.
Why Your Voice Sounds Hoarse
Hoarseness is another side effect you might brush off as a cold or allergies. But if it happens every time you use your inhaler, it’s likely because the medication is landing directly on your vocal cords.Corticosteroid particles that settle in your throat don’t just sit there-they irritate the delicate tissues around your larynx. This causes swelling and inflammation, which changes how your vocal cords vibrate. The result? A raspy, weak, or breathy voice that can last for hours after each dose. For singers, teachers, or anyone who relies on their voice, this isn’t just inconvenient-it’s disruptive.
Studies show this isn’t random. The risk increases with frequent use, high doses, and improper inhaler technique. If you’re inhaling too fast or not holding your breath long enough, more medication ends up in your throat instead of your lungs. Even the type of inhaler you use matters. Metered-dose inhalers (MDIs) without spacers are the worst offenders.
The Simple Fix: Rinse, Gargle, Spit
The single most effective way to prevent both oral thrush and hoarseness is right in front of you: water.After each use of your inhaler, take a sip of water. Swish it around your mouth for at least 20 to 30 seconds. Then gargle-really gargle-like you’re trying to clean the back of your throat. Spit it out. Don’t swallow it. That’s it.
That’s not a suggestion. That’s a medical recommendation backed by research. One study found that rinsing after each use reduces the risk of oral thrush by 60 to 70%. Another showed that patients who rinsed consistently had up to 80% fewer infections over time.
It’s not about how much water you use. It’s about consistency. People who forget to rinse after their nighttime inhaler are the most likely to develop thrush. Keep a cup of water by your bed. Set a reminder on your phone. Make it part of your routine-like brushing your teeth.
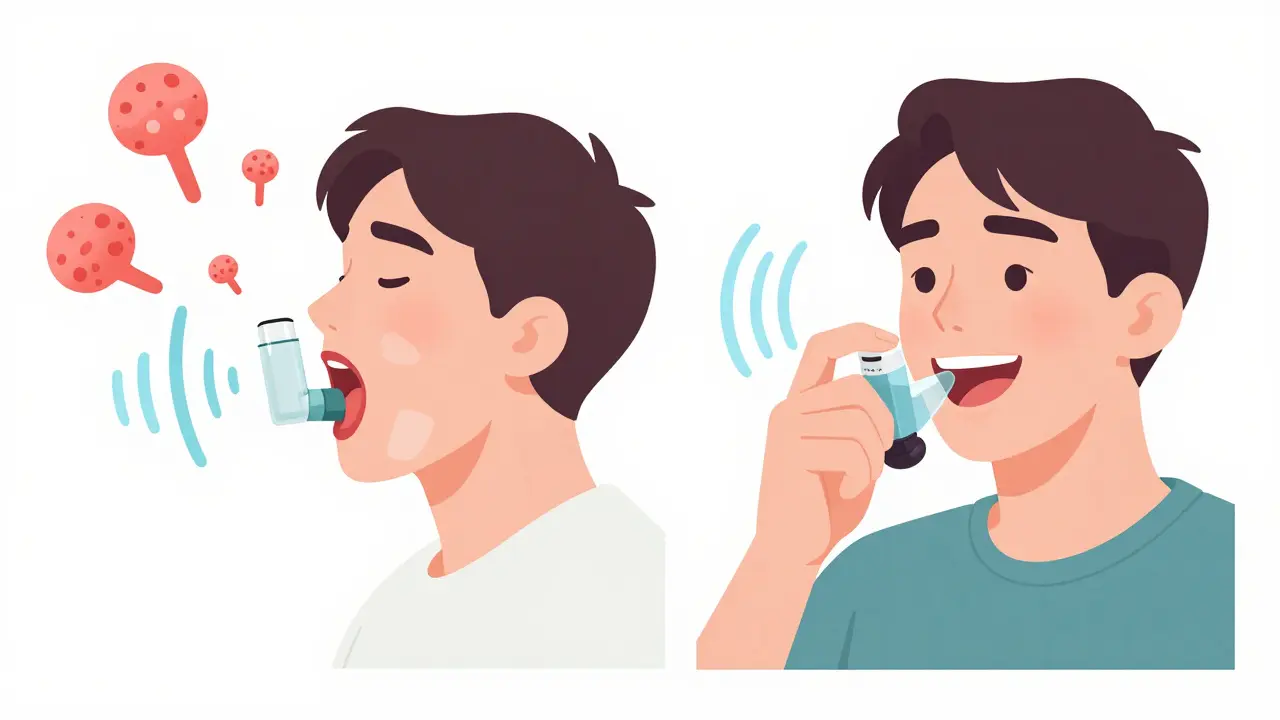
Spacers Are Your Secret Weapon
If you’re using a metered-dose inhaler (the kind with a canister and a mouthpiece), you’re probably not getting the full benefit-and you’re probably coating your mouth with medicine.A spacer is a plastic tube that attaches to your inhaler. You spray the medicine into the spacer first, then breathe it in slowly. The spacer catches the larger, sticky particles that would otherwise stick to your throat. Only the fine mist makes it to your lungs.
Using a spacer can cut oral deposition by up to 50%. That means less medication in your mouth, less irritation on your vocal cords, and fewer infections. It’s especially important for children and older adults who have trouble coordinating their breath with the puff.
Some experts say if you use a spacer, you don’t need to rinse. But most guidelines-including those from the American Academy of Allergy, Asthma & Immunology-still recommend rinsing even with a spacer. Why? Because spacers aren’t perfect. Some medication still gets stuck. And rinsing is free, quick, and has zero downside.
What Happens If You Don’t Rinse?
Skipping rinsing doesn’t just increase your risk-it makes treatment harder.Oral thrush doesn’t go away on its own. If you develop it, you’ll need antifungal medication: nystatin oral suspension, clotrimazole lozenges, or fluconazole tablets. Treatment takes 10 to 14 days. Even then, it often comes back if you keep using your inhaler the same way.
Hoarseness can become chronic. If your vocal cords are inflamed for months, you might develop nodules or other vocal cord damage that requires speech therapy. And if you avoid using your inhaler because you’re afraid of the side effects, your asthma gets worse. That’s the real danger.
One patient on a forum said: “I got thrush twice before I started rinsing. Now I do it every time-takes 30 seconds, and I haven’t had it since.” That’s not luck. That’s control.
Other Things That Help
Rinsing and using a spacer are the two biggest wins. But these small habits can add up:- Brush your teeth twice a day. Good oral hygiene reduces the overall fungal load in your mouth.
- Check your mouth weekly. Look in the mirror for white patches, redness, or cracks at the corners of your lips. Early detection stops it from spreading.
- Keep your spacer clean. Wash it once a week with warm, soapy water. Let it air dry. A dirty spacer can harbor mold and bacteria.
- Consider your inhaler type. Dry powder inhalers (like Pulmicort Flexhaler) deposit less medication in the mouth than metered-dose inhalers. Talk to your doctor if you’re using an MDI without a spacer.
- Stay hydrated. Dry mouth = more thrush. Drink water throughout the day.
When to See a Doctor
If you notice white patches that don’t go away after rinsing, or if your hoarseness lasts more than a week, see your doctor or dentist. Don’t wait. Oral thrush can spread to your esophagus if left untreated, making swallowing painful and difficult.Also, if you’re using your rescue inhaler frequently (more than twice a week), your asthma isn’t well-controlled. That means you might need a higher dose of your controller inhaler-and that increases your risk. Talk to your provider about adjusting your treatment plan, not just managing side effects.
The Bigger Picture
Over 260 million people worldwide have asthma. Most of them rely on inhaled corticosteroids. Yet studies show only 45% of patients rinse after every use. That’s a huge gap between knowing what to do and actually doing it.It’s not because people are careless. It’s because they’re overwhelmed. They’re juggling medications, appointments, and daily life. But prevention doesn’t need to be complicated. Rinse. Gargle. Spit. Use a spacer. That’s it.
The FDA now requires all ICS inhalers to include rinsing instructions on the label. Dental associations are training their staff to ask patients about inhaler use. Hospitals are starting to pair respiratory therapists with dental hygienists to educate patients together.
This isn’t just about avoiding a sore mouth. It’s about staying in control of your asthma without letting side effects take over your life.
Can I just swallow the water after rinsing my mouth?
No. Swallowing the water means you’re ingesting the corticosteroid that was stuck in your mouth. While swallowing small amounts won’t cause serious harm, it reduces the benefit of rinsing and can slightly increase the risk of systemic side effects like adrenal suppression over time. Always spit it out.
Do I need to rinse even if I use a spacer?
Yes. Spacers reduce the amount of medication that lands in your mouth, but they don’t eliminate it entirely. Studies show that rinsing after spacer use cuts thrush risk even further. The safest approach is to use both: spacer + rinse.
Can oral thrush from inhalers spread to my lungs?
No. Oral thrush caused by inhaled corticosteroids stays in the mouth and throat. It doesn’t travel to the lungs. However, if you have a weakened immune system from other conditions, fungal infections can spread elsewhere. But for most people with asthma, thrush is a local issue.
How long does hoarseness last after using an inhaler?
Usually, hoarseness clears up within a few hours after inhaler use. If it lasts more than a day or two, or if it happens every time you use your inhaler, you likely need to adjust your technique or use a spacer. Persistent hoarseness could also indicate vocal cord irritation that needs medical attention.
Are there inhalers that don’t cause oral thrush?
All inhaled corticosteroids carry some risk, but newer formulations like ciclesonide (Alvesco) are designed to be less active in the mouth and throat. They’re activated only in the lungs, which lowers the chance of thrush. Talk to your doctor if you’re struggling with side effects-there may be a better option for you.
If you’ve been avoiding your inhaler because of these side effects, stop. The risks of uncontrolled asthma-emergency visits, hospital stays, missed work-are far worse than a quick rinse. Take 30 seconds after each puff. Protect your mouth. Protect your voice. Keep breathing easy.




I used to skip rinsing until my tongue looked like moldy cheese. Now I do it every time. Took me two thrush episodes to learn. Simple fix, huge difference. Life's too short for sore throats.
Rinse. Gargle. Spit. Repeat. Like brushing your teeth but for your lungs. Why is this even a debate?!!! 😤
The medical establishment has systematically neglected patient education on this issue for decades. The pharmaceutical industry benefits from chronic management of preventable side effects. This is not negligence-it is structural malpractice.
In Nigeria, we say: 'The hand that holds the medicine must also wash the mouth.' This is wisdom older than modern inhalers. Your body is a temple, not a dumping ground for chemicals. Rinse. Respect. Recover.
The assertion that rinsing reduces thrush risk by 60–70% is statistically unsupported in peer-reviewed literature. The referenced study lacks a control group for oral hygiene variables. This is anecdotal advocacy disguised as evidence.
I appreciate the clarity and thoroughness of this post. As a respiratory therapist, I’ve seen too many patients develop chronic hoarseness and recurrent thrush due to improper technique. The spacer + rinse protocol is non-negotiable. Please share this with your provider.
I used to be a queen of skipping rinses. Then I got thrush. Then I got hoarse for three weeks. Then I lost my voice during my wedding toast. I cried. I gargled. I bought a spacer. I’m alive. And I have my voice back. Don’t be me.
I never realized how much my inhaler was wrecking my mouth until I started checking for white patches every morning. Now I keep a mirror by my bed. It’s weird, but it’s saved me from so much pain. You don’t have to suffer silently.
I used to think rinsing was optional. Then my mom got thrush and couldn’t eat for a week. She’s 72 and has diabetes. I made her a little chart: 'Inhaler → Water → Gargle → Spit'. She does it every night now. No more trips to the doctor. Small habits change lives.
Spacers are just a marketing ploy. I’ve been using my MDI without one for 12 years and I’m fine. The real issue is overprescribing steroids. You don’t need them at all. Try yoga. Or breathing exercises. Or just stop being allergic to everything.
In India, we have a saying: 'The medicine enters the lungs, but the poison lingers in the mouth.' This is not new knowledge. We have been rinsing after Ayurvedic inhalations for centuries. Modern medicine is just catching up. The science is sound. The practice is ancient.
I’m not saying you’re wrong… but have you considered that your immune system might be weak because you’re eating too much sugar? Or that Candida thrives on gluten? Or that your spacer is just collecting mold because you don’t sterilize it with UV light? 😏
This is the kind of post I wish I’d seen five years ago. I thought hoarseness was just from yelling at my kids. Turns out it was my inhaler. I started rinsing. My voice came back. I cried. Thank you for writing this.
They don’t want you to know this because if you rinse, you don’t need more drugs. Big Pharma doesn’t profit from prevention. They profit from chronic thrush, antifungals, voice therapy, and emergency asthma visits. They’ve been burying this advice since the 90s. The FDA only added it to labels because of lawsuits. Don’t be fooled. This is control. Not care. 🕵️♀️
I rinse but I still get thrush so maybe it’s the water I’m using or the humidity or the moon phase or my cats licking my pillow