When your kidneys aren’t working right, your body starts to fall out of balance. Too much phosphorus builds up. Fluid piles up in your legs and lungs. Blood clots become more likely. That’s where three key types of medications come in: phosphate binders, diuretics, and anticoagulants. These aren’t optional extras-they’re essential tools to keep you alive and out of the hospital.
Phosphate Binders: Stopping the Silent Threat
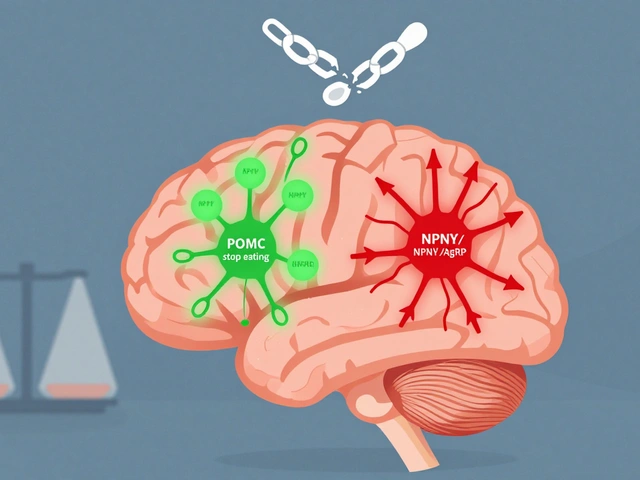
Your kidneys normally flush out excess phosphorus. When they fail, phosphorus builds up in your blood. That sounds harmless, but it’s not. High phosphorus doesn’t just hurt your bones-it hardens your arteries. Studies show that over half of people with late-stage kidney disease have phosphate levels above safe limits. And for every point above 5.5 mg/dL, your risk of heart attack or stroke jumps.
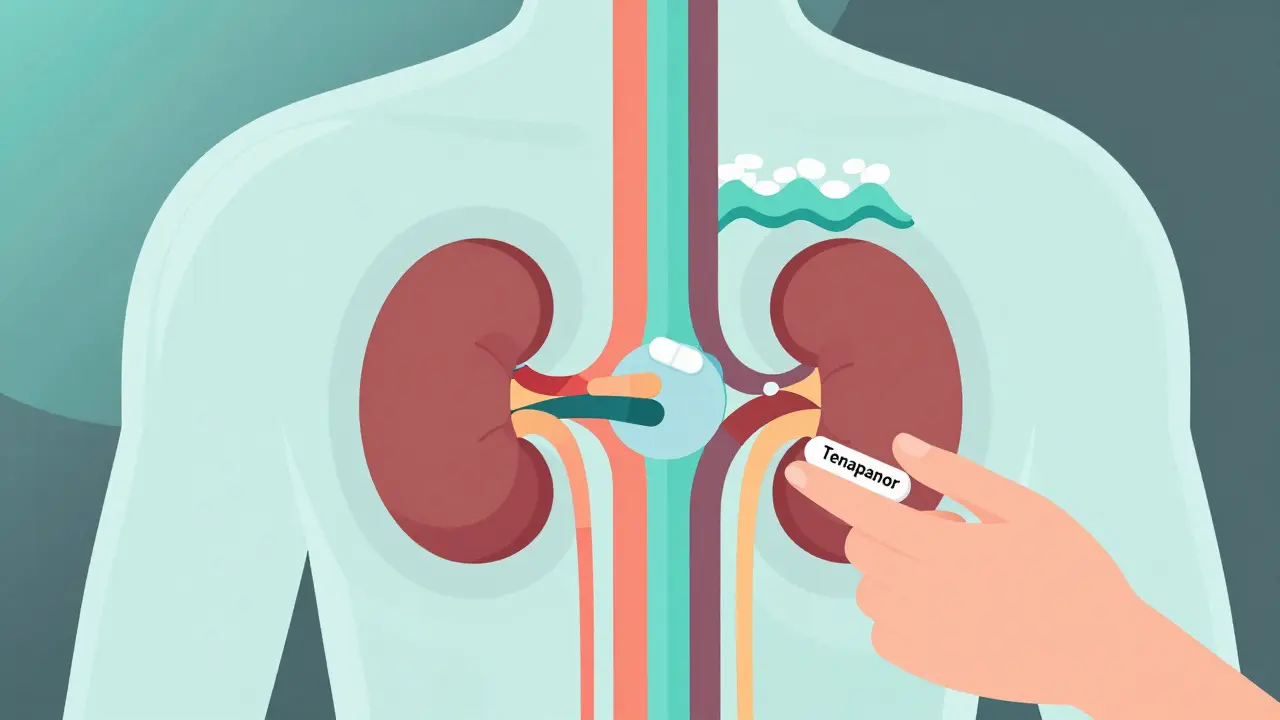
Phosphate binders don’t fix your kidneys. They work in your gut. These pills grab phosphorus from your food before it can be absorbed. You take them with every meal-even snacks. If you skip one, the phosphorus slips through.
There are three main types:
- Calcium-based (like calcium acetate or calcium carbonate): Cheap-often under $80 a month. But they can raise your calcium levels too high, leading to dangerous calcification in your blood vessels. Not ideal if you already have hard arteries.
- Sevelamer (Renagel, Renvela): Costs $150-$250 a month. Doesn’t affect calcium. In fact, studies show people on sevelamer live longer than those on calcium binders. Side effects? Mostly stomach upset and constipation.
- Ferric citrate (Auryxia): Costs about $7,000 a year. It’s newer. It lowers phosphorus and also boosts iron, which helps with anemia. But the price tag makes it unrealistic for many.
One 2022 study found that 68% of patients on sevelamer hit their target phosphate level, compared to just 32% on placebo. But here’s the catch: 42% of people stop taking these pills within six months. Why? Cost, side effects, or just forgetting. The key is consistency. Take them with every bite of food. No exceptions.
Diuretics: Fighting Fluid Overload
Fluid retention is one of the most common reasons people with kidney disease end up in the ER. Swollen ankles. Shortness of breath. High blood pressure. These aren’t just uncomfortable-they’re deadly.
Diuretics, often called water pills, help your body pee out the extra fluid. But not all diuretics work the same in kidney disease.
- Furosemide (Lasix): The old standard. Generic versions cost $4-$10 a month. But in advanced kidney disease, your body stops responding. Up to 60% of patients develop resistance.
- Torsemide (Soaanz): More powerful. 30% better absorbed than furosemide. A 20mg dose equals a 40mg dose of furosemide. It lasts longer, so you don’t need to take it twice a day. Brand name costs $90-$120, but generic is under $25.
- Metolazone: A thiazide diuretic. Useless if your kidney function drops below eGFR 30. But when paired with a loop diuretic like torsemide, it can break through resistance.
The FIRST trial showed torsemide cut heart failure hospitalizations by 22% compared to furosemide. Yet most doctors still start with furosemide-mostly because it’s cheap and familiar. But if you’re in stage 4 or 5 kidney disease, torsemide may be your better bet.
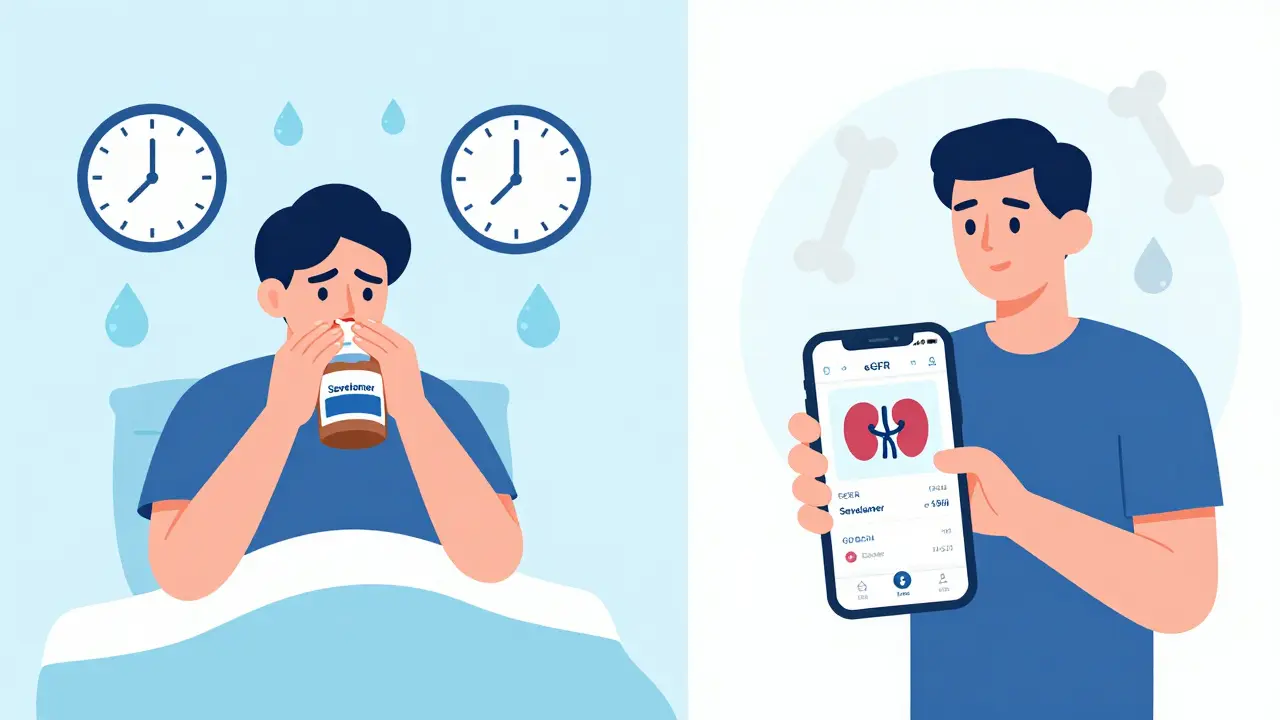
Timing matters. Taking diuretics after 4 p.m. means you’re up all night peeing. Many patients split their dose: two-thirds in the morning, one-third at lunch. That cuts down on sleep disruption without losing effectiveness.
Anticoagulants: Preventing Clots in a Broken System
People with kidney disease have 2 to 4 times higher risk of blood clots and strokes. Why? Damaged kidneys trigger inflammation and clotting. Add atrial fibrillation, and the risk skyrockets.
Anticoagulants thin the blood. But here’s the twist: your kidneys help clear these drugs. So when kidney function drops, the drugs stick around longer. Too much? You bleed. Too little? You clot.
Here’s how the options stack up:
- Warfarin (Coumadin): Old, cheap, and still used. Requires regular blood tests (INR) to check thickness. Surprisingly, it’s more stable in severe kidney disease than newer drugs. Many doctors avoid it, fearing bleeding-but in eGFR under 15, it’s often the safest.
- Apixaban (Eliquis): The top choice for eGFR 15-50. Dose is cut in half (2.5mg twice daily) when kidney function drops. Studies show it causes 31% fewer major bleeds than warfarin. Annual cost: $6,200-$7,500.
- Rivaroxaban (Xarelto): Must be reduced to 15mg daily if eGFR is 15-50. Not approved below eGFR 15.
- Dabigatran (Pradaxa): Higher bleeding risk in eGFR 30-50. Avoid if kidney function is borderline.
- Edoxaban (Savaysa): Not approved if eGFR is below 15. Avoid completely in advanced disease.
The ARISTOTLE trial subanalysis confirmed apixaban’s safety edge. But here’s what most patients don’t know: if you’re on warfarin and your INR is stable, switching to a DOAC isn’t always better. One patient on Reddit said: “Apixaban caused bruising everywhere. Switched back to warfarin. Weekly blood tests are a pain, but I know exactly where I stand.”
Real-World Challenges: Cost, Side Effects, and Adherence
These medications work-but only if you take them.
Phosphate binders? 70% of patients stop taking them within six months. Why? Cost. Nausea. Constipation. The pills are big. You have to take four or five with every meal. It’s a chore.
Diuretics? 68% of patients say frequent urination ruins their sleep. Many stop because they’re too tired of waking up at night.
Anticoagulants? Fear of bleeding. One survey found 28% of CKD patients quit their blood thinners because they were scared of bruising or bleeding.
And cost? Ferric citrate costs $7,000 a year. Apixaban? $7,000. Torsemide? $120 brand, $25 generic. Many patients choose the cheaper option-even if it’s less effective-because they can’t afford the rest.
There’s a tool that helps: the National Kidney Foundation’s “Medicines and CKD” app. It gives real-time dosing advice based on your eGFR. A Mayo Clinic study found it cut medication errors by 27%. If you’re on any of these drugs, download it.
What’s Changing in 2025?
Things are moving fast.
In September 2023, the FDA approved tenapanor (Xphozah). It doesn’t bind phosphate-it blocks its absorption in the gut. Early data shows it reduces phosphate more than sevelamer. Cost? $6,800 a year. Still expensive, but a new option.
The 2024 KDIGO guidelines now say: if you have diabetes and kidney disease, start an SGLT2 inhibitor like dapagliflozin. These drugs reduce phosphate, fluid, and blood pressure-all at once. They may cut your need for phosphate binders by 15-20%.
And research is looking at a new diuretic called AZD9977. Early trials suggest it works even when kidneys are failing. Results are expected in late 2025.
But here’s the truth: no new drug will fix the problem if you can’t afford the one you have now. The real breakthrough isn’t a new pill. It’s better access, better education, and better support.
Bottom Line: What You Need to Do
- If your phosphate is high: Take your binder with every meal. No skipping. If you can’t afford sevelamer, ask about calcium acetate-but get your calcium checked every 3 months.
- If you’re swollen or short of breath: Ask your doctor about switching from furosemide to torsemide. Split your dose. Don’t take it after 4 p.m.
- If you have atrial fibrillation: Apixaban is your best bet if your eGFR is above 15. If it’s below 15, warfarin may be safer. Never stop your anticoagulant without talking to your nephrologist.
- Use the NKF app. It’s free. It saves lives.
Kidney disease doesn’t have to be a death sentence. But these medications? They’re not optional. They’re your shield. Take them right. Monitor them. Ask questions. And don’t let cost or side effects stop you from living.




Yo this is actually one of the clearest breakdowns I’ve seen on kidney meds. I’ve been on torsemide for 8 months now and honestly? Life-changing. Used to be up 5x a night. Now I sleep like a rock. Also switched from calcium binders to sevelamer after my doc finally listened. My phosphorus dropped from 7.1 to 4.8. No more bone pain. Don’t let cost scare you-ask for samples, patient programs, even generic ferric citrate if you’re anemic. You’re not alone.